Home, Search, Index, Links, Pathology, Molecules, Syndromes,
Muscle, NMJ, Nerve, Spinal, Ataxia, Antibody & Biopsy, Patient Info
|
Home, Search, Index, Links, Pathology, Molecules, Syndromes, Muscle, NMJ, Nerve, Spinal, Ataxia, Antibody & Biopsy, Patient Info |
|
Acromegaly Adrenal Carcinoid myopathy Corticosteroid Diabetes Gonadal Dysgenesis Gynecomastia Hypogonadism Insulinoma Parathyroid Hyperparathyroid Hypoparathyroid Thyroid Hyperthyroid Hypothyroid |
 From Bramwell: Atlas of Clinical Medicine Myxedema
|
|
Hyperthyroid Myopathy Ophthalmopathy Other associated disorders Hypothyroid Adult Childhood Other associated disorders External link: Testing |

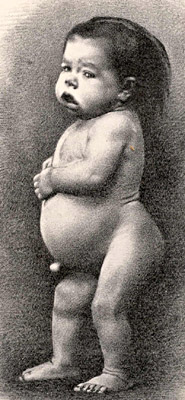 From Bramwell: Atlas of Clinical Medicine |
|
|
|
Epidemiology Myopathy Ophthalmopathy Other Associated disorders |
|
|
|
Adrenal insufficiency Corticosteroid-binding globulin deficiency Corticosteroid myopathy Corticosteroid withdrawal Myosin loss myopathy Nelson |
 Cushing 1912 Cushing's Syndrome
("Pluriglandular Syndrome") |
|
||||||||||||||||||||||||||||||||||||||||||
Corticosteroid myopathy
|
|
|
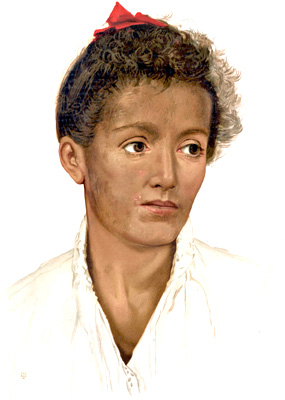 From Bramwell: Atlas of Clinical Medicine Addison's Disease
|
|
|
||||||||||||
|
|