Home, Search, Index, Links, Pathology, Molecules, Syndromes,
Muscle, NMJ, Nerve, Spinal, Ataxia, Antibody & Biopsy, Patient Info
|
Home, Search, Index, Links, Pathology, Molecules, Syndromes, Muscle, NMJ, Nerve, Spinal, Ataxia, Antibody & Biopsy, Patient Info |
|
Generalized Drugs Myopathic Non-muscle disorders Polymyalgia Localized Cramps: Differential diagnosis Pain medications Principles Pain Muscle pain Also see Painful neuropathies |
| MUSCLE DISCOMFORT ± MYOPATHY: DRUGS & TOXINS | ||||
|---|---|---|---|---|
| Inflammatory Myopathy |
Rhabdomyolysis & High CK ± Chronic myopathy |
Painful myopathy ± Rhabdomyolysis |
Myalgia ± Myopathy |
Cramps |
|
Definite Hydralazine Penicillamine Procainamide L-tryptophan (impurity) Possible Cimetidine Interferon-α Ipecac Leuprolide Levodopa Penicillin Phenytoin Propylthiouracil Proton pump inhibitors Sulfonamide |
Alcohol e-Amino Caproic Acid Amphetamines Anti-Psychotics Loxapine Quetiapine Cocaine Cyclosporine Hypokalemia Isoniazid Lipid lowering agents Fibrates Bezafibrate Clofibrate Gemfibrozil Statins Lovastatin Simvastatin Pravastatin Fluvastatin Atorvastatin Cervistatin Red yeast rice Lithium Mibefradil Neuroleptic-Malignant Propofol Zidovudine |
Colchicine Emetine Germanium Hypervitaminosis E Taxenes Zidovudine |
All-Trans-Retinoic Acid Azathioprine Bryostatin 1 Captopril Ciguatoxin Corticosteroids Withdrawal Cytotoxics Danazol Enlapril Gemcitabine Gold Interferon α-2a Interferon α-2b Isotretinoin Ketorolac Labetalol Methotrexate Metolazone Mycophenolate mofetil Neuropathy: Small fiber Paclitaxel Retinoids Rifampin Spanish toxic oil Suxamethonium (Succinylcholine) Tyrosine kinase inhibitors Vinca alkaloids Zimeldine |
Albuterol Anti-Cholinesterase Bergamot (bergapten) Caffeine Clofibrate Cyclosporine Diuretics Labetalol Lithium Nifedipine Terbutaline Tetanus Theophylline Vitamin A |
|
Afferent neurons & axons Primary (PNS) Secondary (CNS) Descending pathways Pain perception Sensory terminals Nociceptor (axon) types Stimulus types Acid Chemical Temperature Mechanical Sensitization |
|
Peripheral sensitization Central sensitization |
| Mechanism | Symptom | Molecular targets | Drugs |
|
Na+ channels Accumulation Redistribution Altered expression |
Spontaneous pain Paresthesias Neuroma sign |
Na+ channels TTX-sensitive TTX-resistant |
Carbamazepine Lamotrigine Mexilitine Tricyclic antidepressants |
| Central sensitization |
Hyperalgesia Tactile Cold Pin-prick |
NMDA receptors Neurokinin-1 receptors nNOS Protein kinase γ |
NMDA antagonists Ketamine Dextramethorphan Amantidine |
| Peripheral sensitization |
Hyperalgesia Pressure Thermal Spontaneous pain Neurogenic inflammation |
Vanilloid receptor-1-desensitization Neurokinin 1 Na+ channels: TTX-resistant Nerve growth factor |
Capsaicin |
| Sympathetic stimulation |
Spontaneous pain |
α-receptor antagonists Nerve growth factor/trKA |
Phentolamine Guanethidine |
| Increased transmission Reduced inhibition |
Spontaneous pain Hyperalgesia |
Calcium channels, N-type Receptors |
Conotoxin Opiates Gabapentin Clonidine Tricyclic antidepressants SNRIs |
|
Causes Drug-induced Features Basic Clinical |
Delayed Onset Muscle Soreness (DOMS)
6
|
|
| Diagnostic Criteria (Healy) |
Persistent pain (> 1 month) involving two of : neck, shoulders, pelvic girdle Morning stiffness (> 1 hour in duration) Abrupt onset of illness (< 2 weeks) Age: ≥ 50 years Erythrocyte sedimentation rate > 40 mm/hr Rapid response to prednisone (≤ 20 mg/day) Absensce of other disorders |
|
|
|
|
| Bergamot oil 8 |
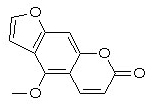 Bergapten
|