NEUROMUSCULAR DISEASE: TYPICAL PATTERNS
GENERAL PRINCIPLES
- Clinical patterns:
- General: The neuromuscular evaluation
- Begins with: Evaluation & description of patterns of disease process
- Gleaned from: History & physical examination
- Unusual patterns
- Especially important
- Provide basis for listing most likely diagnoses
- Summary of disease syndrome should include features from each descriptive category
- Function patterns
- General Most useful for differential diagnosis when selective involvement occurs
- Motor
- Weakness
- Muscle size
- Abnormal movements
- Sensory
- Loss: Large or Small fiber modalities
- Discomfort
- Autonomic
- Anatomic patterns
- Arms vs. Legs vs. Cranial
- Most neuromuscular disorders: More prominent in legs early in disease course
- Neuromuscular junction disorders: Cranial weakness early
- Proximal vs Distal
- Symmetric vs Asymmetric
- Symmetric disorders are more common
- Asymmetric neuropathies
- Commonly treatable
- Often related to immune disorders
- Nerve biopsy often indicated
- Selective regions involved in: Neuropathy or Myopathy
- Temporal patterns
- Course
- Acute: Days to Weeks
- Chronic: Months to Years
- Episodic
- Hereditary: By family history or examination of relatives
- Fatigue: Over course of minutes to hours
- Onset age
- Tissue & Anatomic involvement
|
|
|
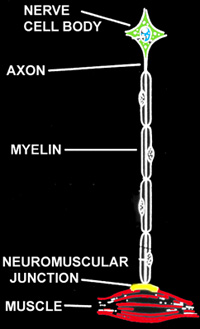
Loci of NM Disease
Tissue & Anatomic
|
- Diagnostic (Molecular) testing: When a pattern of disease
and its tissue localization are identified other laboratory testing can be employed
to make a specific diagnosis, guide consultation of the patient, and
direct treatment. Diagnostic tests include:
- Muscle biopsy
- Histochemistry: Diagnosis by specific morpholgic features
- Immunohistochemistry: Absent or reduced staining for specific protein
- Biochemistry: Absent or reduced enzyme function
- Ultrastrucure: Rarely helpful
- Nerve biopsy
- Antibodies
- Location: Serum or CSF
- May define specific immune neuromuscular disorders
- Genetic testing: May define specific hereditary disorders
MUSCLE
Other laboratory tests
NEUROMUSCULAR JUNCTION
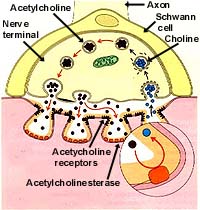
|
|
Normal neuromuscular junction
|
- Clinical patterns of disease
- Weakness
- Distribution
- Proximal & Distal
- Extraocular muscles & Face: Often involved
- Cause: NMJs of extraocular muscles have
different anatomy & physiology
- Temporal changes: Variable through day; Fatigue
- Sensory: Normal
- Tendon reflexes: Normal
- Cause: No involvement of sensory axons
- Electrophysiology
- Repetitive nerve stimulation
- Normal: No change in amplitude of compound motor action potentials (CMAPs)
- Neuromuscular junction disorders: Altered CMAP amplitude with repeated stimulation
- Decrement
- Anatomy: Post-synaptic disorders
- Due to reduced safety factor at synapse
- Increment
- Anatomy: Pre-synaptic disorders
- Due to altered release of vesicles from pre-synaptic terminal
- EMG & Nerve conduction testing: Normal
- Other laboratory tests
- Antibodies (serum) vs
- Rule out associated disorders
- Paraneoplastic screen: Rule out
- Thyroid function testing: Myasthenia gravis
- Muscle biopsy
1890 illustration
of upper and lower
motor neurons by
Ramon y Cajal
|
NERVE
Cell body
- Clinical patterns of disease
- Functional involvement
- Often largely one modality
- Distribution
- Proximal & Distal
- Arms: Involved early
- Face & Bulbar: Common
- Asymmetric
- Time course
- Onset frequently subacute: Weeks to months
- Defect very persistent & poorly responsive to therapy
- Electrodiagnostic
- Selective loss of motor, sensory, or autonomic axons
- Early involvement of proximal structures
- Motor: Thoracic paraspinous muscles denervated
- Sensory: Truncal sensory loss
- Cause: Cell body pathology is not dependent on axon length
- Other laboratory tests
- Pathology: Loss of cell bodies
- Antibodies: Immune disorders
- Genetic evaluation: Often with positive family history
Myelin
- Clinical patterns of disease
- Weakness: Proximal & Distal
- Wasting: Not prominent unless concomitant axonal loss
- Sensory loss
- Mild
- Symmetric
- Distal > Proximal
- Tendon reflex loss
- Diffuse
- Early in disease course
- Causes: Demyelination
- Occurs all along length of axons: No selective proximal or disat involvement
- Produces asynchronous conduction of sensory stimuli to motor cell bodies
- Depolarization of motor cell does not reach threshhold for generating action potential
- Nerve conduction studies
- Conduction velocity: Slow
- Upper extremity velocities: < 32 M/s
- Distal latencies & F-waves: Prolonged
- Conduction block: Failure of impulse conduction along an anatomically intact axon
- Cause of abnormalities: Disordered saltatory conduction of impulses along axons
- Other laboratory tests
Axon
- Clinical patterns of disease
- Weakness
- Distal
- Legs > Arms
- Muscle wasting: Early
- Cause: Rapid muscle fiber atrophy after denervation or disuse
- Sensory
- Loss
- Distal > Proximal
- Legs > Arms
- Modalities: Vibration loss > Proprioception loss; Pain & Temperature
- Discomfort
- Paresthesias & Pain
- Distal > Proximal
- Legs > Arms
- Cause: Spontaneous action potentials from damaged small axons
- Tendon reflex loss
- Electrodiagnostic studies
- EMG
- Motor unit pathology
- Pattern: High amplitude, Prolonged, Polyphasic, Rapid firing
- Cause: Increased number of muscle fibers in each motor unit due to axonal sprouting
- Spontaneous activity
- Anatomic invlolvement
- Distal > Proximal
- Legs > Arms
- Cause: Longer axons often more vulnerable to disease process
- Nerve conduction studies
- Small compound motor action potentials
- Conduction velocities: Mildly slowed (Upper extremity > 35 M/s)
- Other laboratory tests
- Biopsy
- Genetics: Most useful with positive family history
|