General
- Drug properties
- Action
- Inhibits acetylcholinesterase
- Prolongs presence of neurotransmitter, acetylcholine, in the NMJ
- Results in enhanced muscle strength
- Duration: Lasts for a few minutes
- Response
- In patients with NMJ dysfunction
- Not specific for MG
- Time course: Minutes; Rapid-onset; Short-acting
Method
- Initially
- Dosing: 2 mg of edrophonium is administered intravenously as a test dose
- Monitoring heart rate: Bradycardia or ventricular fibrillation may develop
- Follow-up
- After observing for about 2 minutes, if no clear response develops
- Up to 8 additional mg of edrophonium is injected
- A double-blind protocol with a saline injection as placebo has been advocated
- Testing performed with patient free of all cholinesterase-inhibitor medications
- Cholinergic side effects of edrophonium
- May include
- Salivation & Lacrimation: Increased
- Sweating & Flushing
- Bladder urgency
- Fasciculations, perioral
- Atropine should be readily available
- To reverse effects of edrophonium if hemodynamic instability
- Extra precautions: Especially important in elderly patients
Positive test
- Most myasthenic muscles respond in 30 to 45 seconds after injection
- Improvement in strength that may persist for up to 5 minutes
- Requires objective improvement in muscle strength.
- Do not over interpret
- Subjective or minor responses: Reduction of sense of fatigue
Utility of Tensilon test
- Only useful in patients with objective, preferably measurable, findings on physical examination
- Rarely helpful in the diagnostic evaluation of equivocal cases of MG
- Sensitivity for MG is relatively low (60%) compared to other diagnostic tests
- Tensilon testing should not be used to determine adjustments in the dose of pyridostigmine
- False positive results
- Can occur in patients with LES, ALS or even localized, intracranial mass lesions
- Positive testing does not necessarily predict respose to a longer-acting anti-AChE drug
|
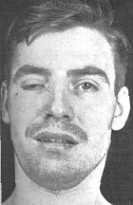

Cogan
|
|
Tensilon test: Before (left); After (right)
|
|