FOCAL MYOSITIS
2
- Epidemiology
- Onset Age
- Range: Childhood to 70's
- Common: Adulthood; Most in 30's to 50's
- Sex: Male = Female
- Identical twins: 1 set both with disease
- Local pain
- Clinical features
- Muscle mass
- Solitary (Asymmetric)
- Pain: 14% to 81%
- Enlarging (Days to Months)
- Size: 1 to 20 cm
- Quality: Firm; Dense; Tender
- Muscles involved
- General
- Distribution: Legs (70%); Arms (22%); Head & Neck (8%)
- 1 (62%) to 3 contiguous muscles
- Leg: Quadriceps; Gastrocnemius
- Also: Abdomen; Arm; Forearm; Neck
1; Paraspinous; Tongue; Perioral
- May involve: Whole, or region, of one muscle or several adjacent muscles
- Erythema (40%)
- Associated disorders
- Immune syndromes (32%); Behcet (5%)
- Neoplasms (24%)
- No generalized weakness
- No joint involvement
- Natural history
- Self limited course: Months; < 4 years
- Eventual spontaneous regression
- Recurrence
4: 1% to 41%; May occur in other muscles
- Reported prior events: Campylobacter; Borrellia burgdorferi; BCG vaccination
- Differential diagnosis: Nodular fasciitis; Sarcoma; Proliferative myositis
- Treatment
- Control pain & inflammation: Analgesics & NSAIDS
- Corticosteroids: 0.75mg/day for 3 to 12 weeks
- Physical therapy to reduce contracture
- ? Surgery
- Laboratory
- Serum CK
- Normal (80%)
- If high: Increased frequency of developing more diffuse involvement
- Dysglobulinemia (50%): Polyclonal gammopathy
- Inflammatory markers: Some patients; ESR high, CRP high, ANA+
- EMG: Myopathy + Spontaneous activity in affected muscle
- CT: Poorly defined enlargement; Fatty infiltration; No discrete mass
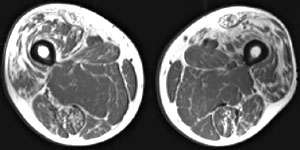
- MRI: Muscle enlargement; Edema (High T2 signal; Low T1 signal); Circumscribed mass
- Ultrasound: Normal orientation of muscle fibers
- Muscle pathology
- Perimysial & Endomysial connective tissue: Thickened
- Myopathic changes: Varied muscle fiber size; Internal nuclei; MHC1 up
- Inflammation: T-cell predominant
- Distribution: Varied within muscle
- HLA types: A2, B62, Cw3 & DQ3 common to small series of Japanese patients
- Differential diagnosis
- Benign tumors
- Rhabdomyoma, Fibromatosis, Intramuscular lipoma
- Malignant tumors
- Not restricted to single muscle
- Rhabdomyosarcoma, Liposarcoma, Leiomyosarcoma, Metastasis
- Vascular intra-muscular tumor
- Inflammatory myofibroblastic tumors
- Lymphoma
- Proliferative myositis
- Myositis ossificans
|

From M. Al-Lozi
MRI: T2 weighted image
|
Focal myositis
Brachialis (Arrow)
|
|