Dural:Type I; Extramedullary
5
- Anatomy & Physiology
- Location
- Thoracic (Lower) & Lumbar: 90%
- Sacral: 4%
- Cervical 3%
- Left > Right: 2:1
- Feeding vessels
- Location: Often lumbar
- Number: Usually 1; Occasionally 2 or 3
- Fistula in dorsolateral root sleeve
- High venous pressure in spinal cord
- Reduced spinal cord perfusion
- Epidemiology
- Male:Female = 4:1
- Age of onset: Mean 58 years; Range 21 to 78
- 75% of all AVMs
- Clinical
- General
- Lumbar or sacral signs most common
- Poor correlation between lesion & level of symptoms
- Similar syndrome: Associated with remote pelvic AVM
- Initial symptom
- Gait disorder
- Sensory symptoms: Numbness or Paresthesias
- Pain (low back, or radicular)
- Leg weakness: Often asymmetric
- No change with Valsalva
- Hemorrhage: 5% to 25%
- Sensory
- Loss: Sacral 1st; Spinal level in 20%
- Paresthesias
- Pain: Back or Legs; 25% to 50%
- Motor
- Weakness
- Legs: Mild paraparesis most frequent
- May be asymmetric
- Progression to flaccid
- Lower motor neuron only in 35%
- Wasting: Proximal - buttocks & thighs
- Gait disorder
- Early in course: Exacerbated by exercise
- Later in course: Fixed
- Reflexes
- Tendon: Reduced or increased
- Plantar: Upgoing
- Anal & cremasteric: Reduced
- Bladder dysfunction
- Frequency: 80%
- More severe with conus AVM
- Vascular
- Bruit: Rare
- Cutaneous angioma
- More prominent with Valsalva
- ? Related to dural or intradural AVM
- Progression
- Gradual over months to years
- Short term exacerbations: Related to exercise
- Stepwise exacerbations: 20%; Related to ischemia or hemorrhage
- Full symptom complex (motor, sensory, bladder) after 1 year in 2/3
- Severe gait disorder: 90% by 3 years
- Treatment
6
- Endovascular
- Surgery
- Cut intradural venous connection to parenchyma
- Improvement in 60% to 80%
- Symptom recurrence may be 2° to new collaterals to AVM
- Benefit
- Motor & gait improvement most likely: Rarely reverts to normal
- Pain often reduced
- More improvement with lower thoracic AVMs
- Diagnosis
- Myelography: 90% positive
- MRI
7
- Use small field of view
- Eliminate motion artifact
- T2 signal or flow voids: Present in most
- Perform T1 sequence after gadolinium: Detects enhancement
- 86% positive
- Detects other lesions
- Spinal angiography7
- Localizes fistula
- May be only positive diagnostic test (30% to 50%)
|

From M Al-Lozi
Arteriogram:
Tortuous vessels
|
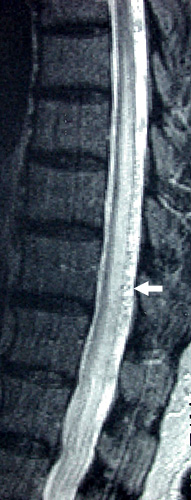
MRI T2:
Flow voids on dorsal cord surface
|

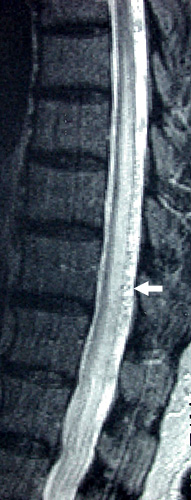
MRI T1:
High signal in cord
|