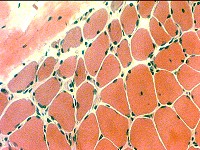
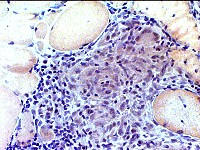
H & E stain
Answer: Perifascicular atrophy of muscle fibers
What other structure is commonly damaged in these regions?
Answer: Capillaries are damaged and lose their endothelium.
What is the most likely diagnosis?
Answer: Dermatomyositis with vascular pathology
This is the typical pathology seen in children, and some adults, with dermatomyositis.
There is muscle fiber atrophy and vacuolarization but little necrosis
It differs from another type of dermatomyositis (IMPP) that has
Damaged perimysium with histiocytic (Acid phosphatase-positive) cellularity
No capillary pathology.
Strong associations with: Interstitial lung disease; tRNA synthetase antibodies
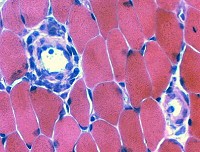
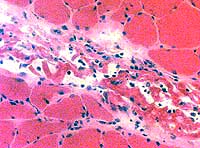
H & E stain
Answer: Mononuclear cell infiltrate around an intermdiate-sized blood vessel
The perivascular infiltrate is suggestive of an immune disorder.
There is no damage to the vessel wall that would suggest a vasculitis.
There are no myopathic changes to support a diagnosis of myositis.
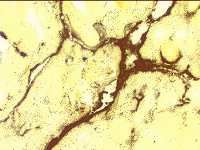
Alkaline phosphatase stain
How would you interpret this pattern of abnormality?
Answer: Alkaline phosphatase staining of perimysium supports
a diagnosis of an immune mediated, often treatable, myopathy
What other patterns of abnormal alkaline phosphatase staining occur in muscle?
Answer: Alkaline phosphatase staining
Around the rim of muscle fibers: Muscle fiber necrosis
Capillaries near regions of perifascicular atrophy: Common in childhood dermatomyositis
Muscle fiber cytoplasm: Immature or regenerating muscle fibers
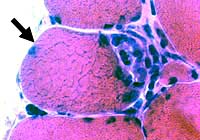
H & E stain
Answer: Focal invasion of muscle fiber by inflammatory cells
How would you interpret this finding (focal invasion)?
Answer
Focal invasion of muscle fibers can occur in both Polymyositis and Inclusion body myositis.
The finding does not distinguish between treatable myositis and untreatable IBM-like disorders
What other stains might be performed to clarify the disease process?
Answer
Cells invading muscle fibers are commonly labeled by: Acid phosphatase and Non-specific esterase.
Evaluation for IBM-like disorders: Congo red for vacuoles; SMI-31 for aggregates
Congo red stain
Answer: Granuloma
There are multinucleated giant cells
What additional stains would be useful to confirm your impression?
Answer: Esterase and Acid phosphatase will stain most of the histiocytic cells in the center of granulomas
Giant cell markers are: Lysozyme; α1-antichymotrypsin Small dark cells surrounding the histiocytic cells, and often extending into the endomysium. are lymphocytes.
H&E stain
Answer: Perimysial damage, Often immune-mediated
What additional stains would be useful to confirm your impression?
Answer: Perimysial cellularity often stain with Esterase and Acid phosphatase.
What is a differential diagnosis for this pattern of pathology?
Answer: Acid phosphatase-positive cellularity in the perimysium commonly occurs in
Fasciitis (Immune or Toxic).
Immune myopathies with perimysial pathology (IMPP)
IMPP syndromes are multisystem disorders.
Other systems often involved include skin (Dermatomyositis subtype) and lungs (Interstitial lung disease).
Graft-vs-Host Disease
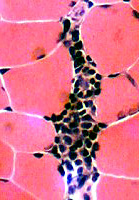
H&E stain
What does this pattern of inflammation suggest?
Answer: The dark mononuclear cells are probably lymphocytes forming a lymphorrhage.
What additional tests would be useful to confirm your impression?
Answer: Repetitive nerve stimulation; Anti-AChR antibodies; Chest CT
Esterase stain showed small, multifocal neuromuscular junctions.
The patient had myasthenia gravis and thymoma.