DERMATOMYOSITIS: Childhood & Adults
2
Dermatomyositis with Vascular Pathology (DM-VP)
|
DM-VP Childhood Muscle fiber pathology Aggregates (LC3) Vacuoles MHC Class I Perifascicular atrophy Borderzone Epimysial Stains Gomori trichrome H&E NADH Mitochondrial Alkaline phosphatase MxA Toluidine blue Vessel pathology Capillaries, Endomysial H&E stain Alkaline phosphatase Complement deposition Endothelial stains Ulex Immunohistochemistry Ultrastructure Artery & Vein, Perimysial Damage Inflammation Variants Adult Child, Severe DM syndromes, Other IMPP RIIM |
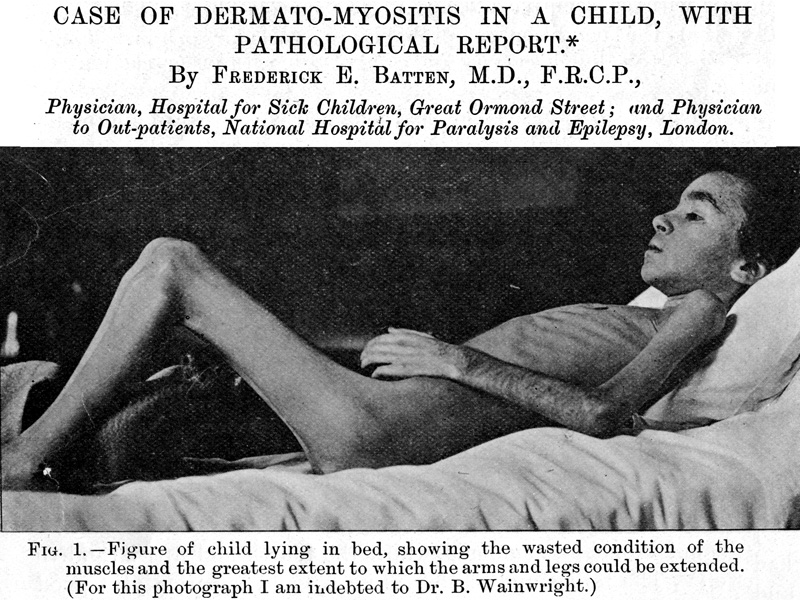 Br J Child Dis 1912;9:247 |
Dermatomyositis with Vascular Pathology (DM-VP)
Muscle fiber atrophy: Perifascicular (Border zone) distribution
- Atrophic muscle fibers: Patterns
- Location
- Border zone regions of vascular supply
- Edge of fascicles: Near
- "Avascular" perimysium
- Edge of muscle (Epimysium)
- Morphology
- Internal architecture: Abnormal
- Not necrotic
- Location
- Muscle fibers, Abnormal: Pathology
- Morphology
- Internal architecture: NADH
- Mitochondrial pathology
- Aggregates
- Nuclei in small muscle fibers: Enlarged; Commonly internal
- Necrotic and regenerating fibers: Rare
- More common in: DM-like disorders in adults (IMPP)
- Muscle fibers in regions near perimysial vessels: Larger or normal
Original Pathologic Description of Dermatomysitis with Vascular Pathology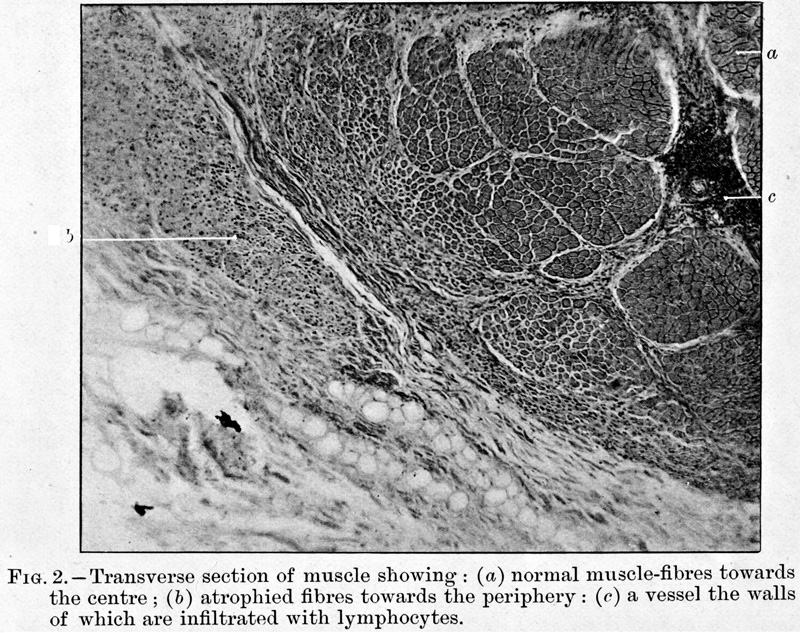 Batten FE Br J Child Dis 1912;9:247 |
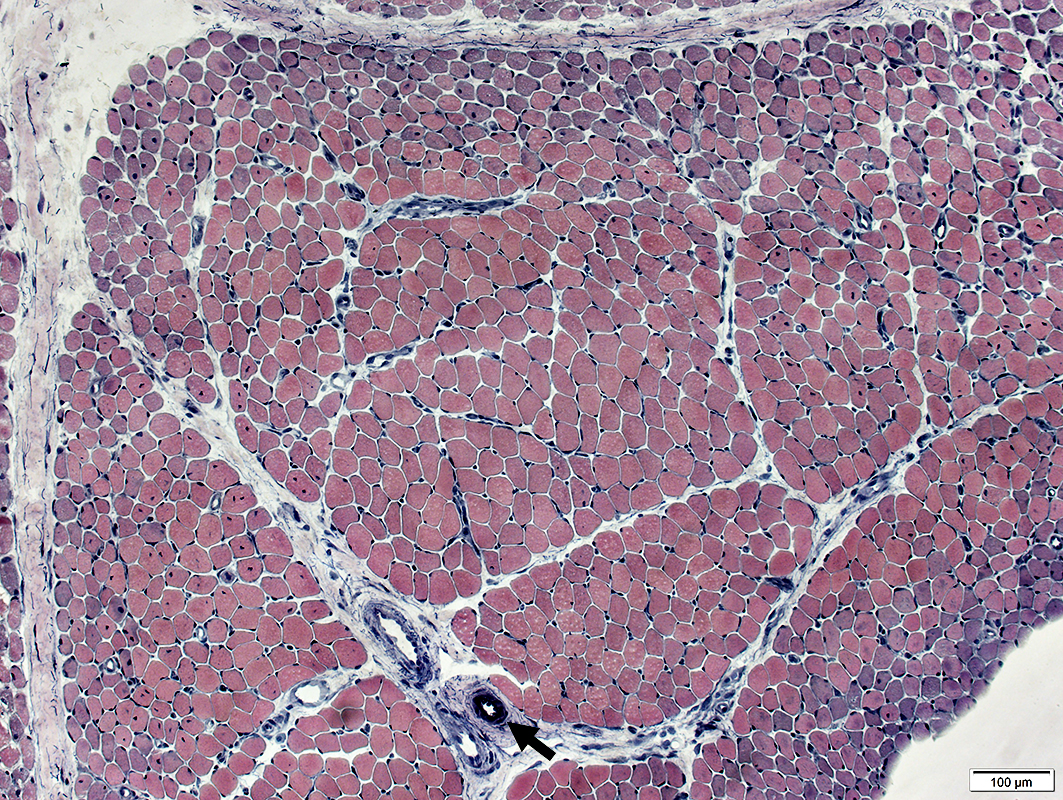
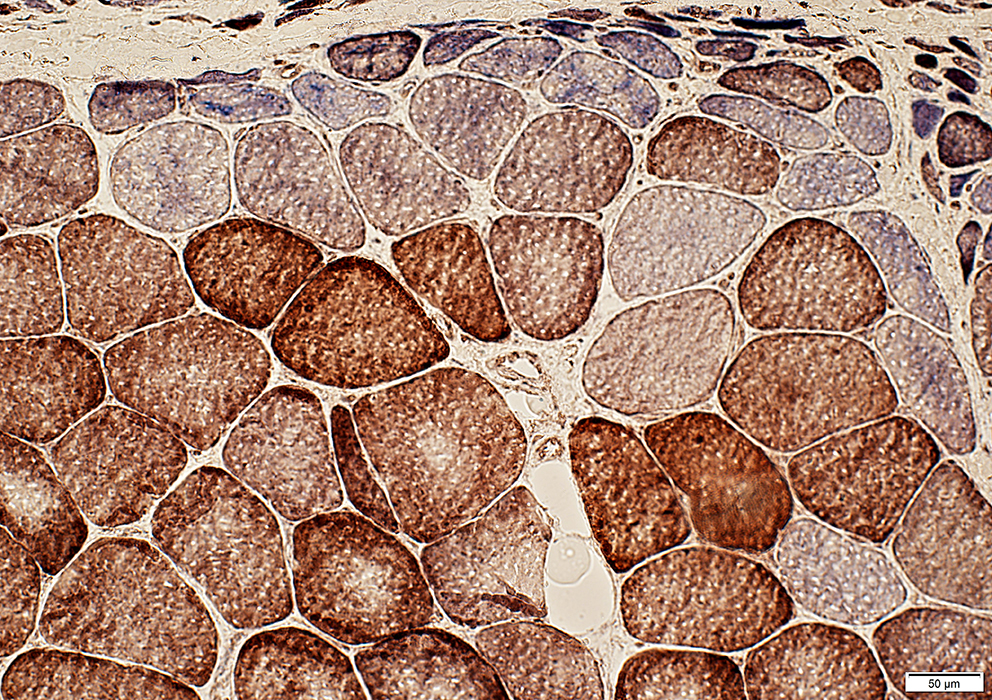
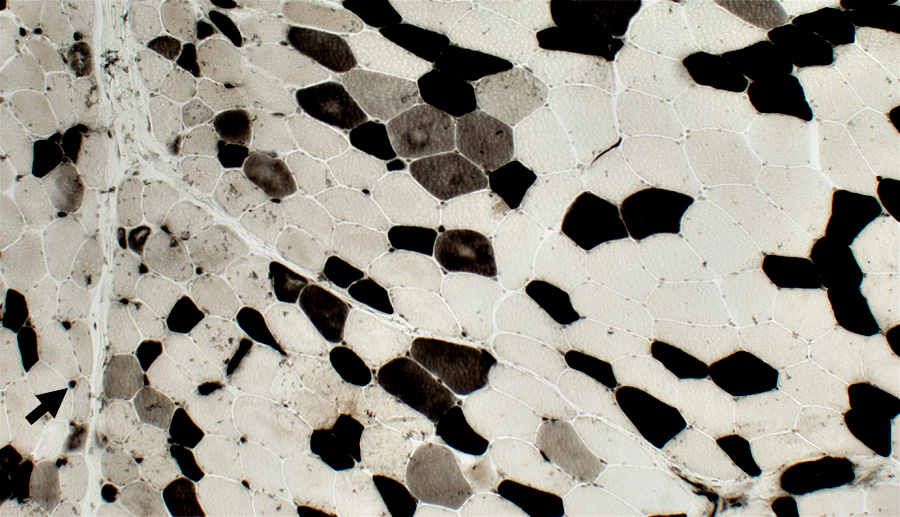
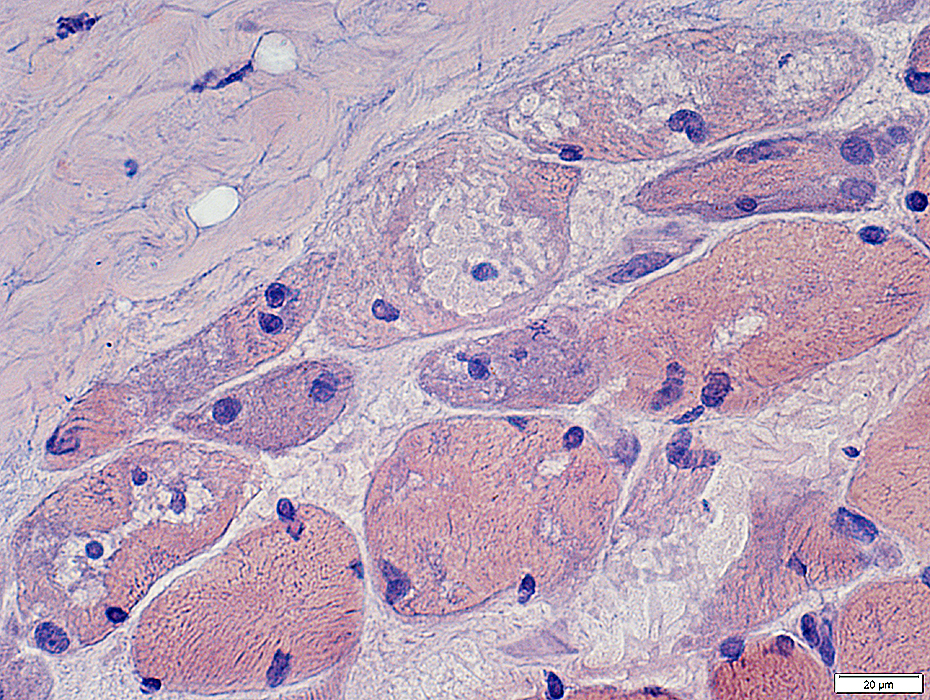
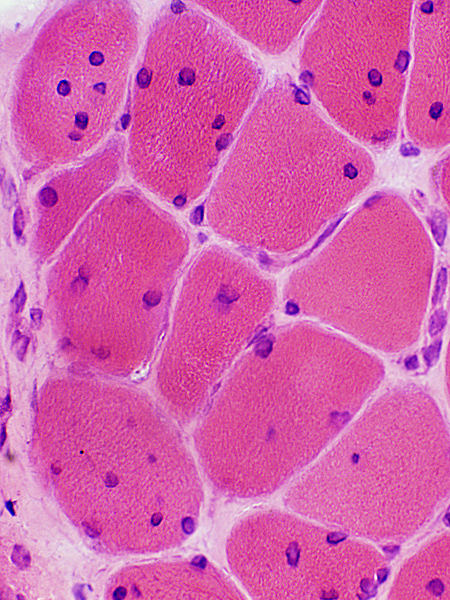
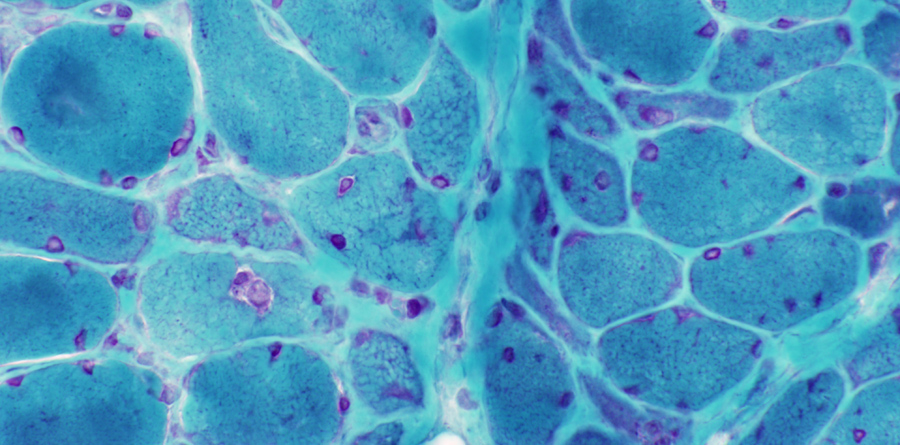
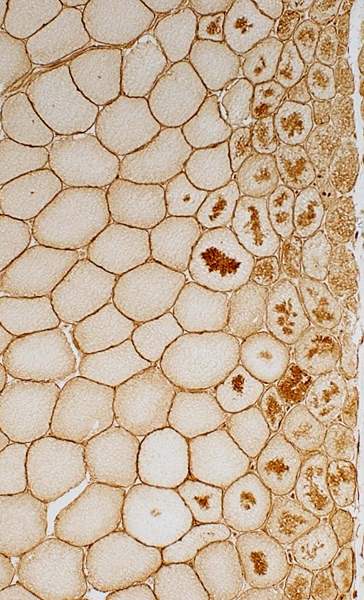
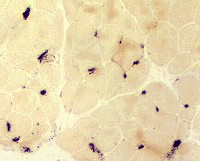
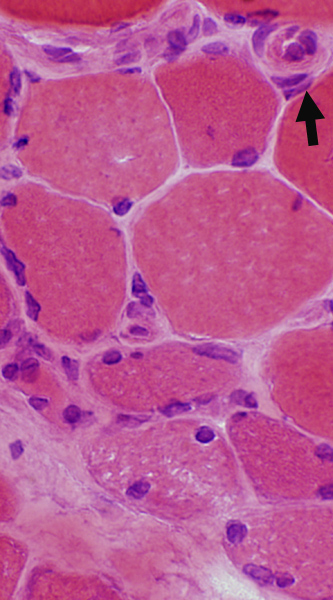
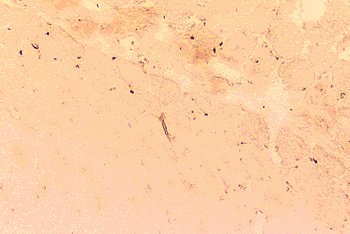
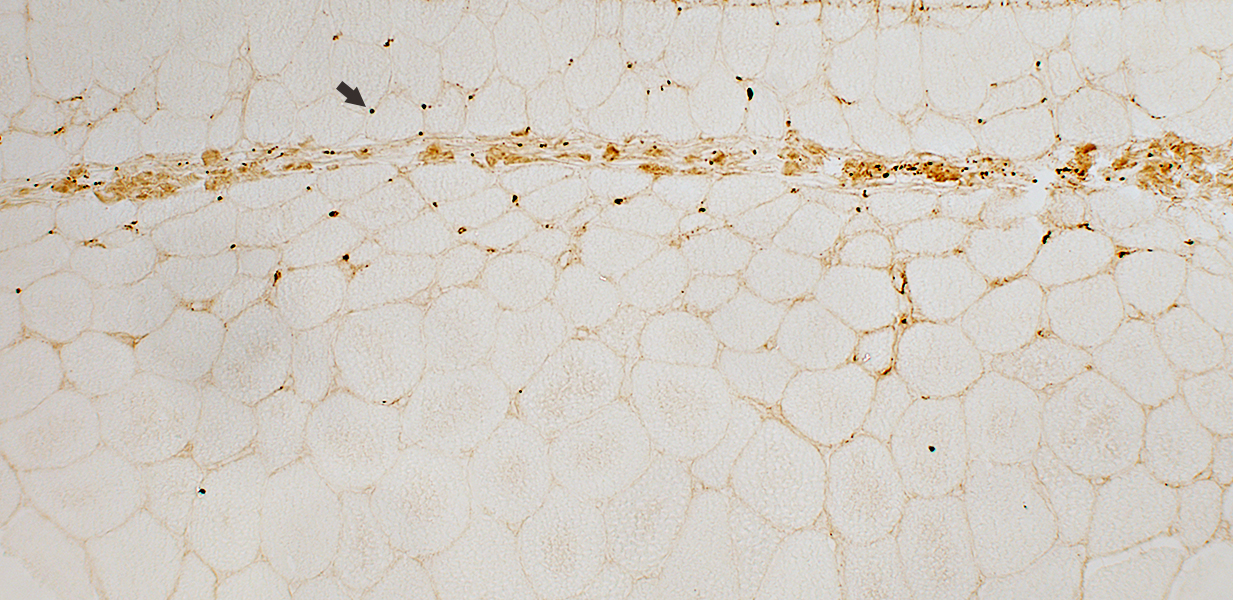
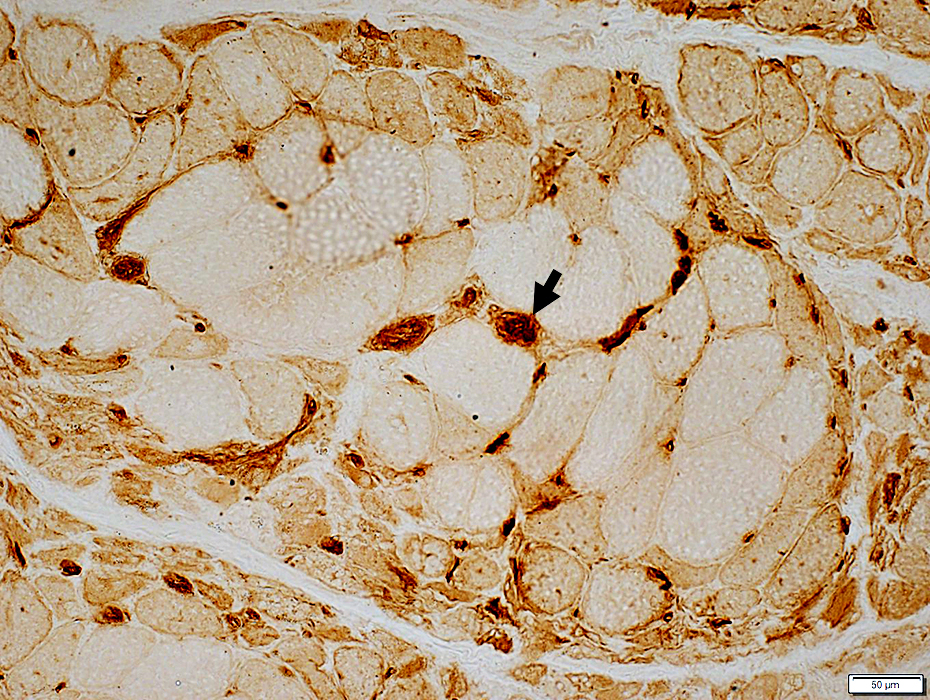
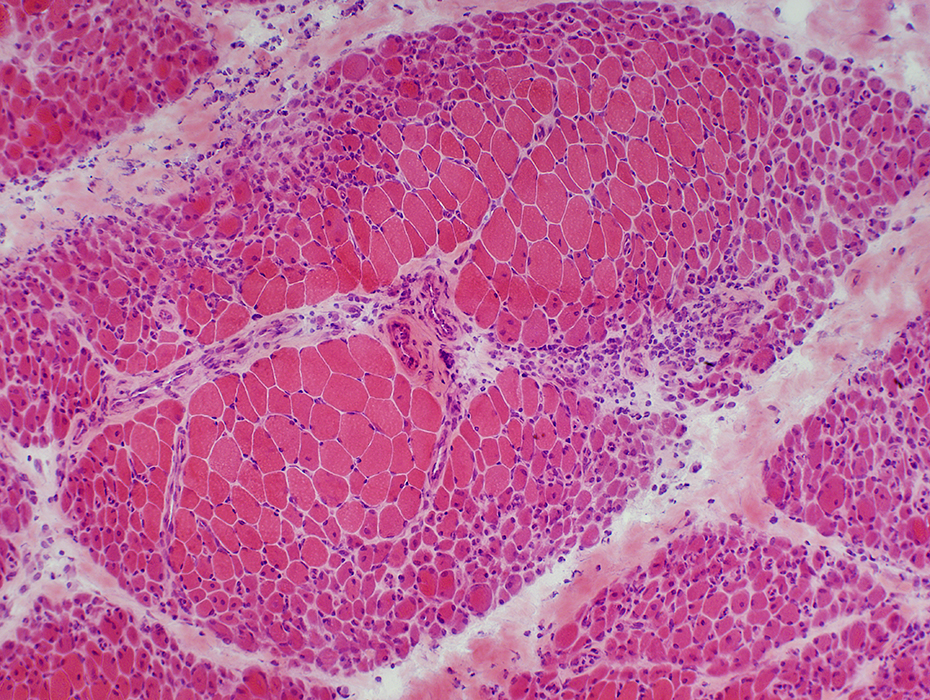
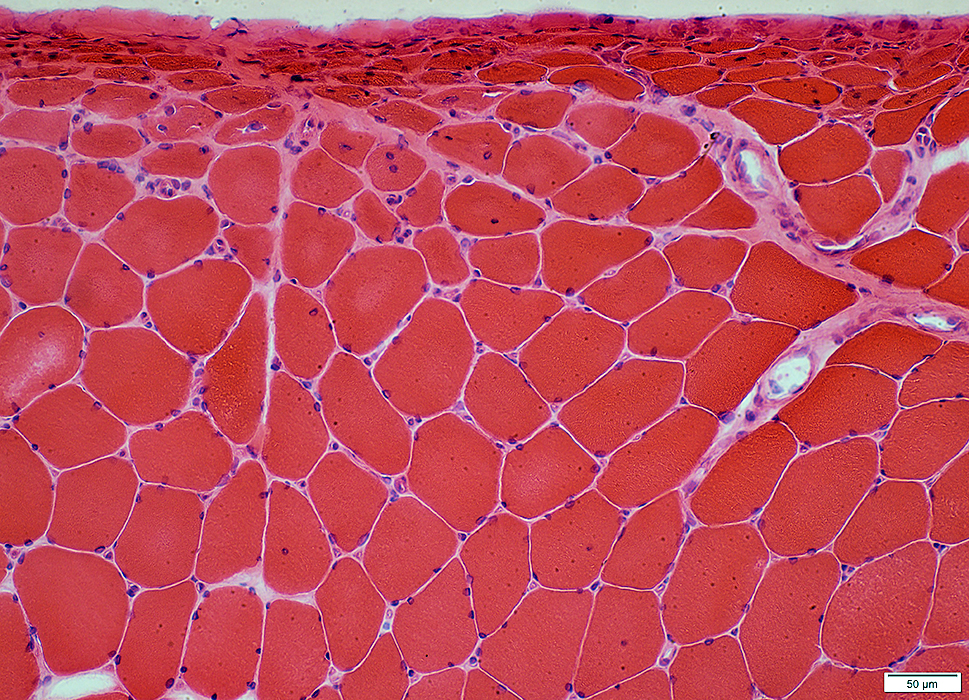
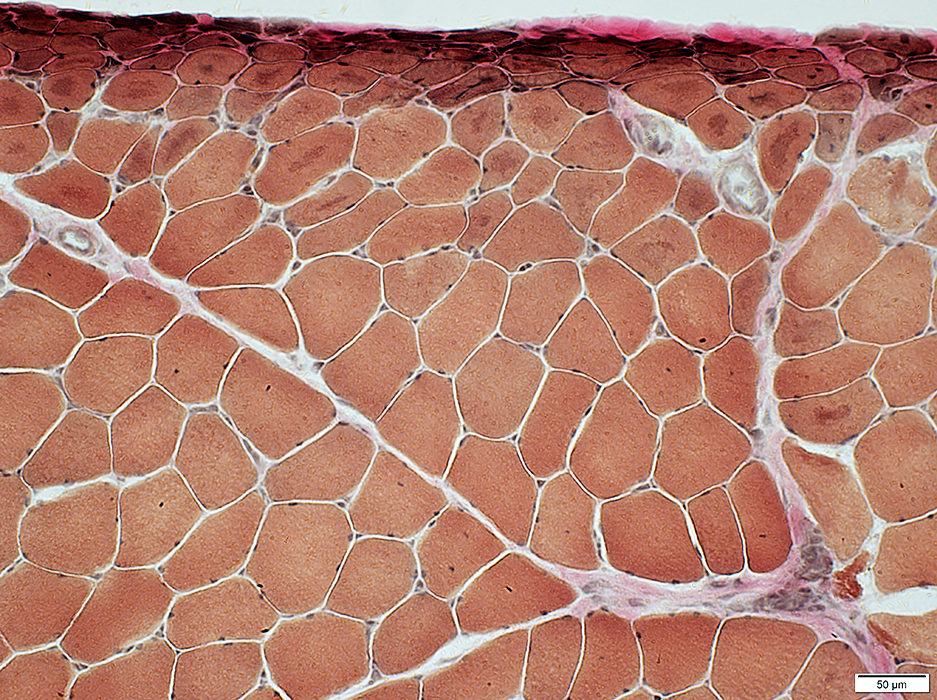
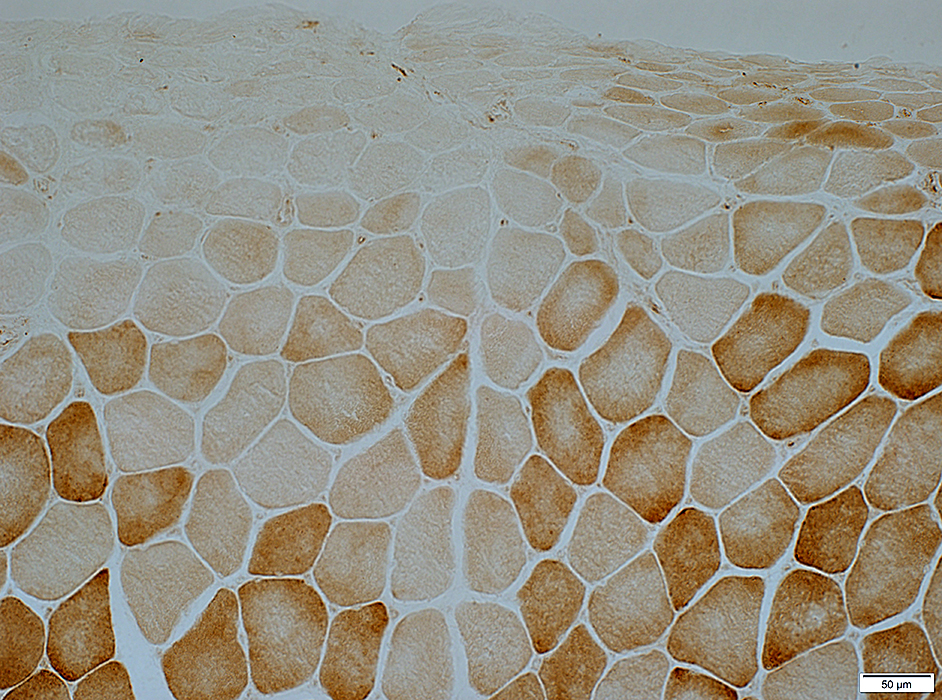
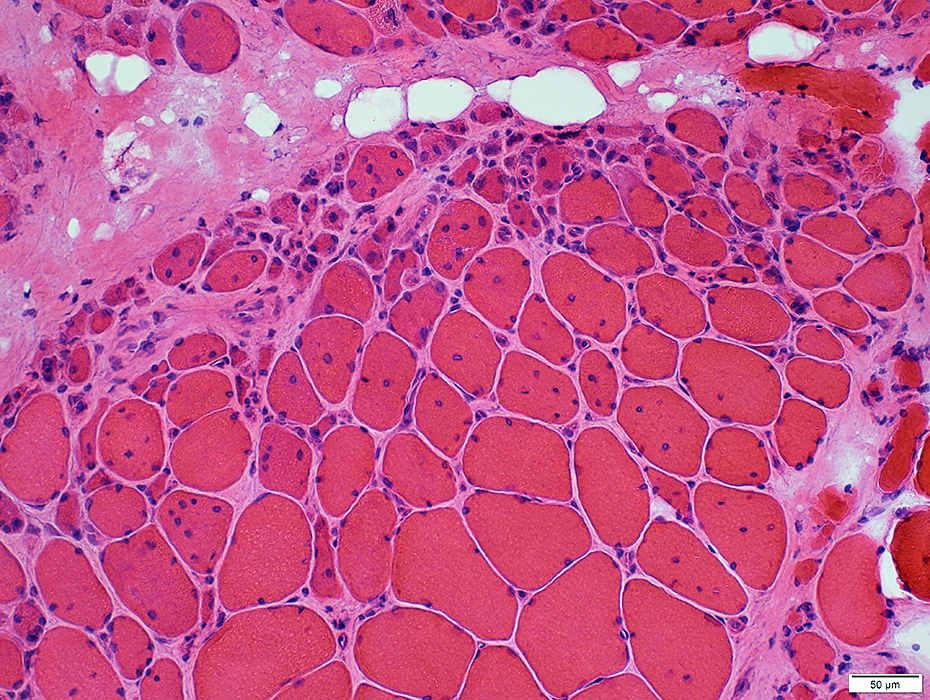
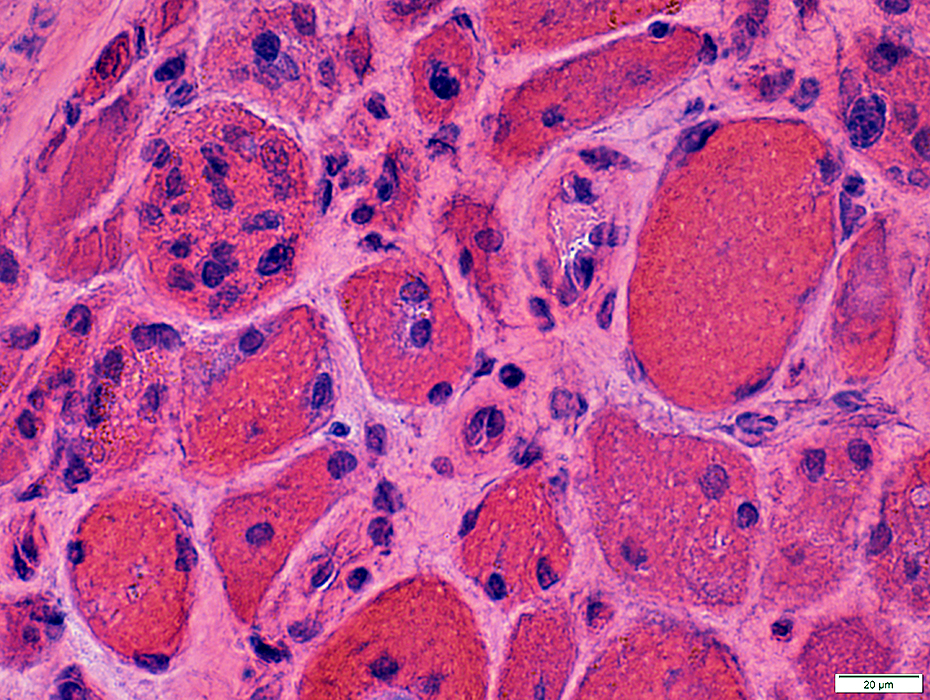
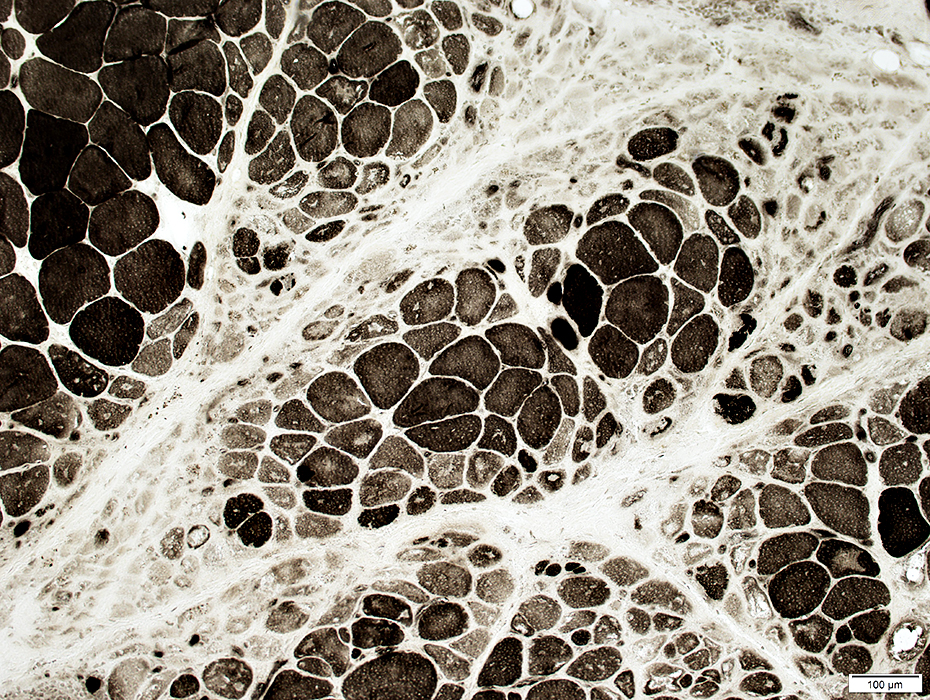
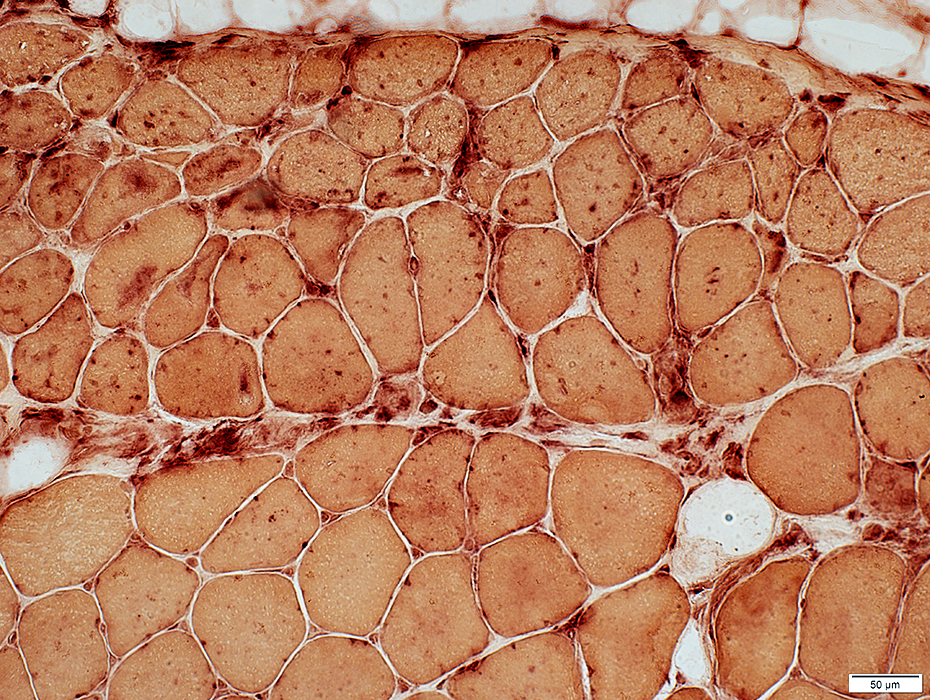
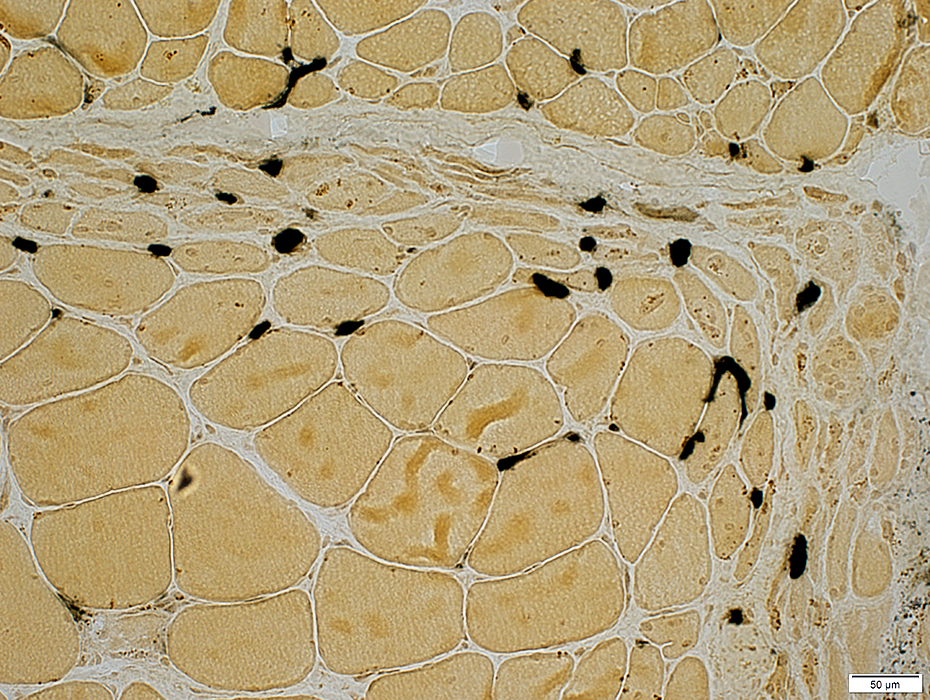
DM-VP: Perifascicular Muscle Fiber Smallness
Atrophic Muscle Fibers: Near Avascular Perimysial Connective tissue (Dark arrow) surrounding fascicleLarger Muscle fibers: Within fascicle near intermediate sized perimysial vessels
Vessel in Vascular Perimysium: White Arrow
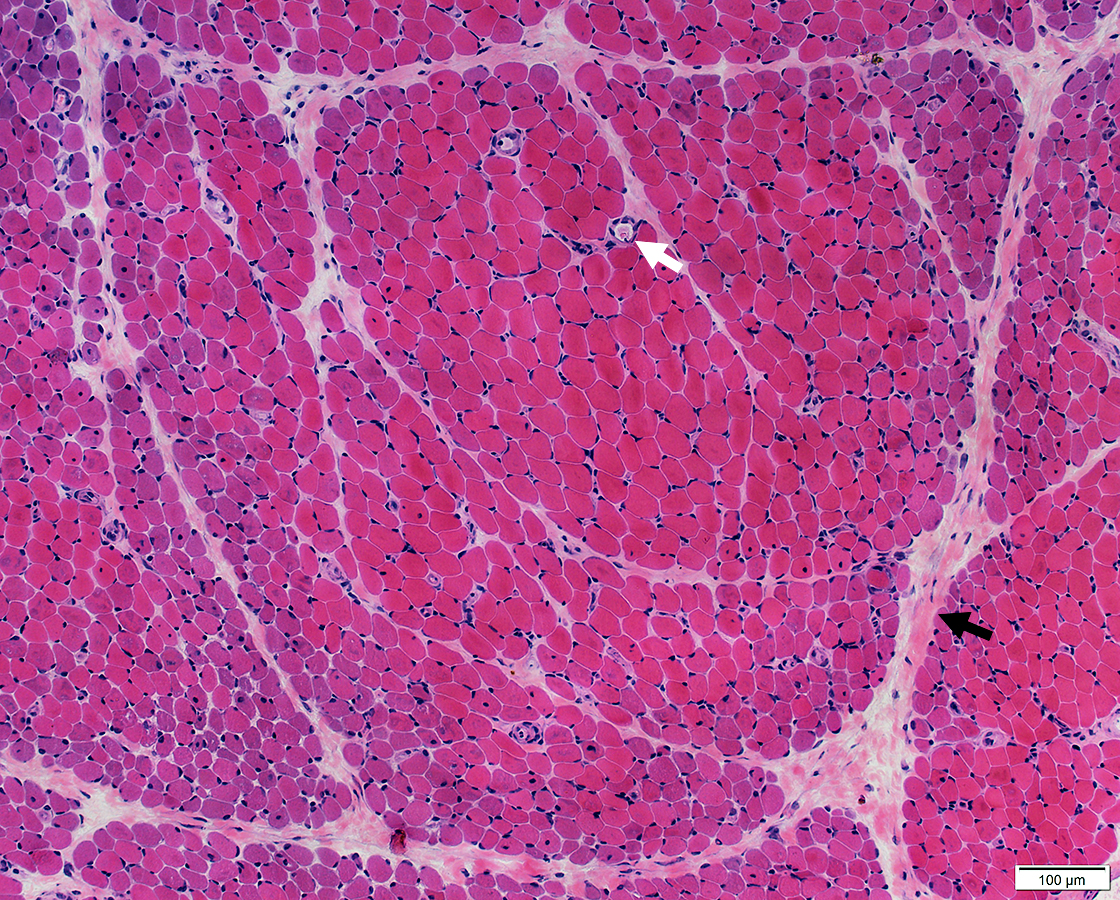 H&E stain |
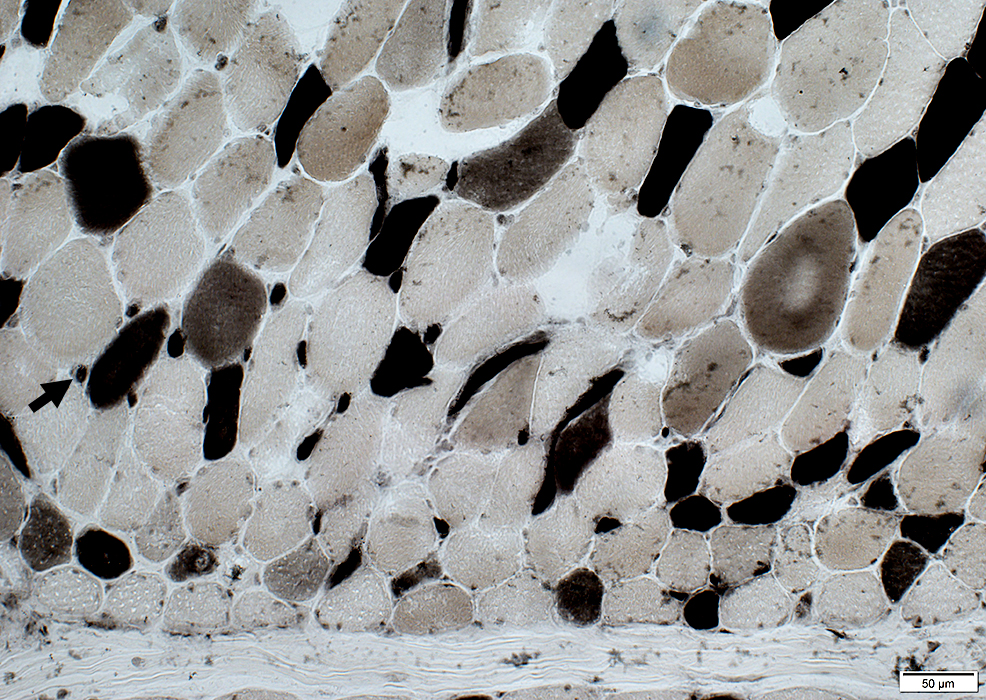
Border-zone Muscle Fiber PathologyPerifascicular Muscle Fiber Atrophy: Along Avascular PerimysiumAtrophic perifascicular muscle fibers neighbor a long region of avascular perimysium (Center). Normal sized muscle fibers neighbor vascular perimysium (Sides). Control: Vessels & Perimysium 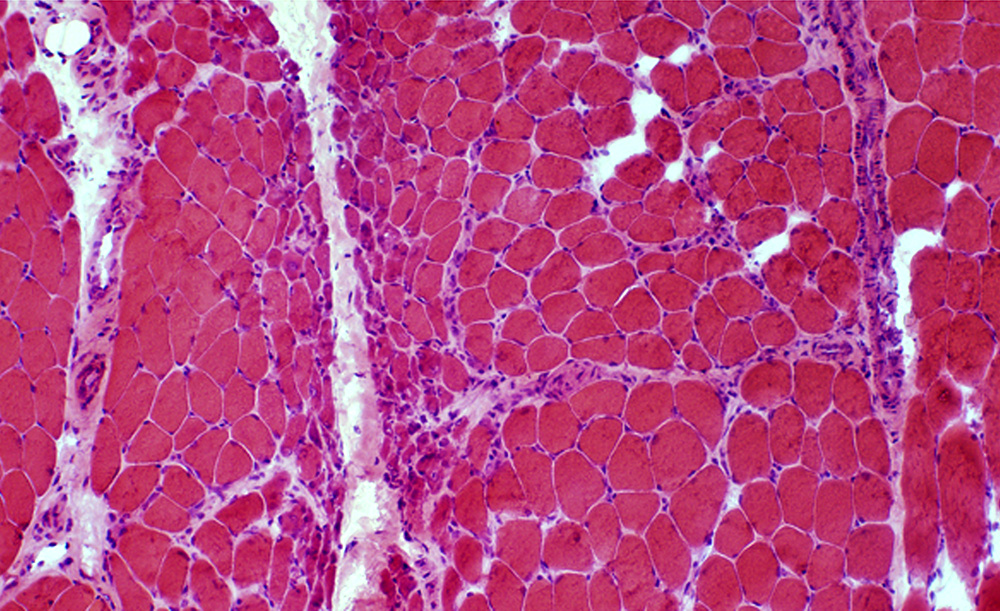 H&E stain |
Vessels & Vascular Perimysium: Within fascicle, Within region containing larger muscle fibers (Dark Arrow)
Avascular Perimysium: Neighbors small muscle fibers (Top & Left)
 VvG stain |
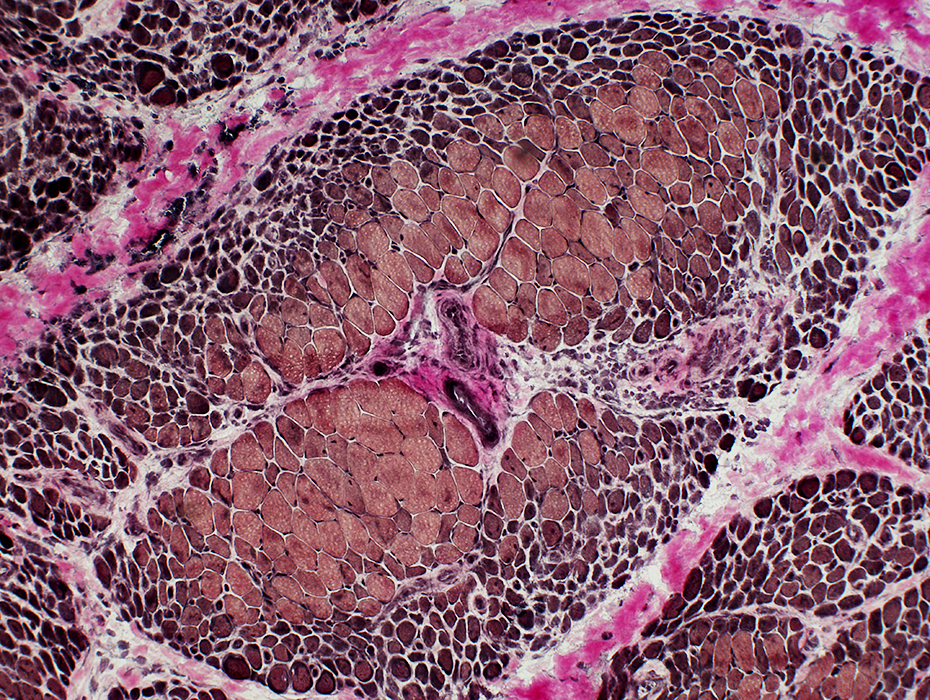
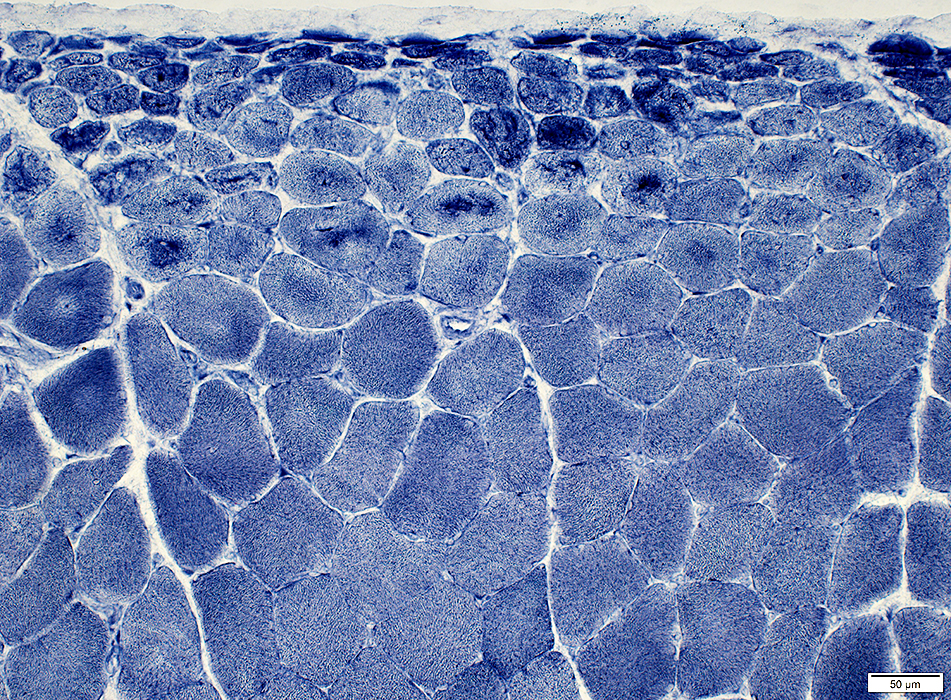
Vessels & Vascular Perimysium: Within fascicle, Within region containing larger muscle fibers (Dark Arrow)
Avascular Perimysium: Neighbors small muscle fibers (Surrounding perimysium)
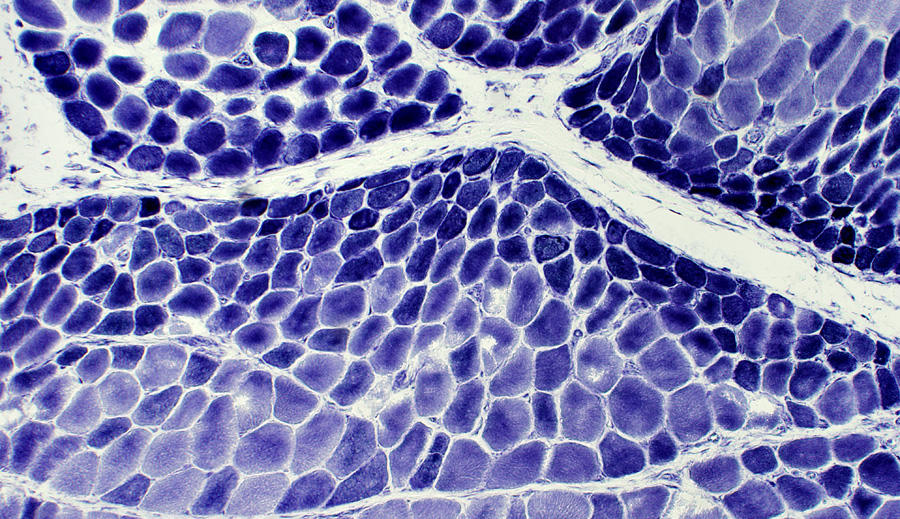
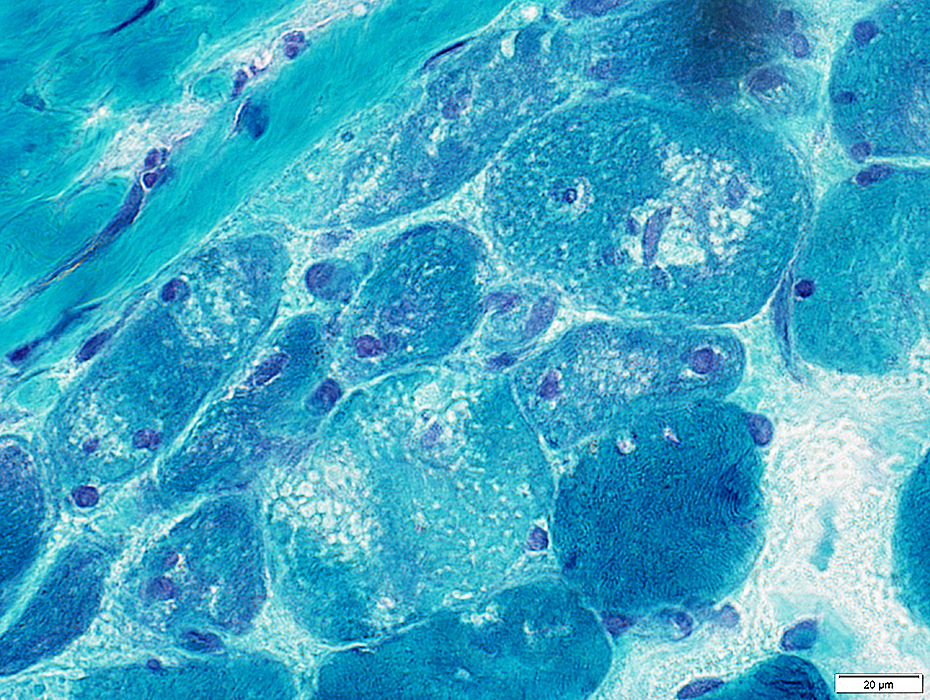
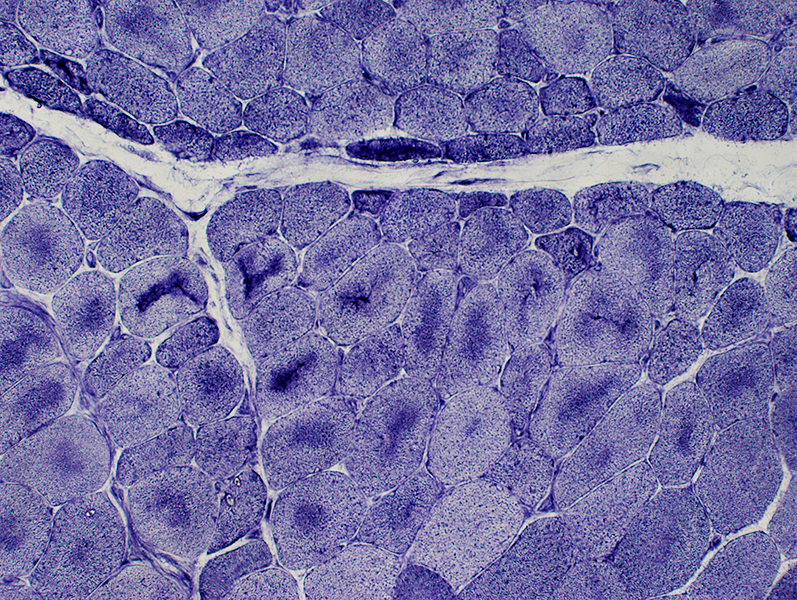
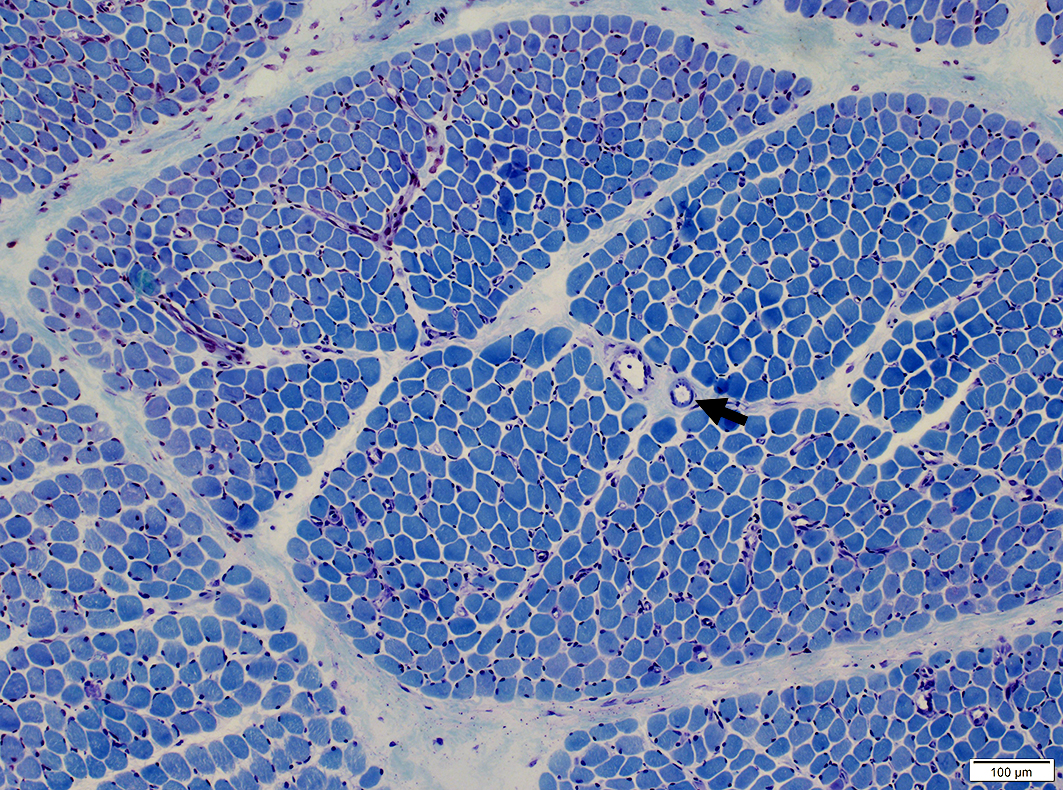 Toluidine Blue stain |
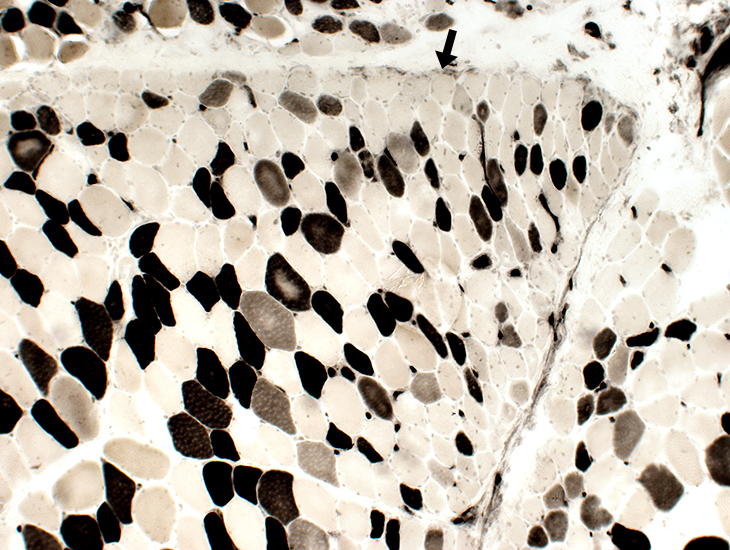
Vessels & Vascular Perimysium: Within fascicle, Within region containing larger muscle fibers (White Arrow)
Endomysial capillaries: Abnormal ATPase staining in areas near muscle fiber atrophy
Avascular Perimysium: Neighbors small muscle fibers (Surrounding perimysium) (Dark Arrow)
Small muscle fibers near edge of fascicle: Often type 2 or 2C
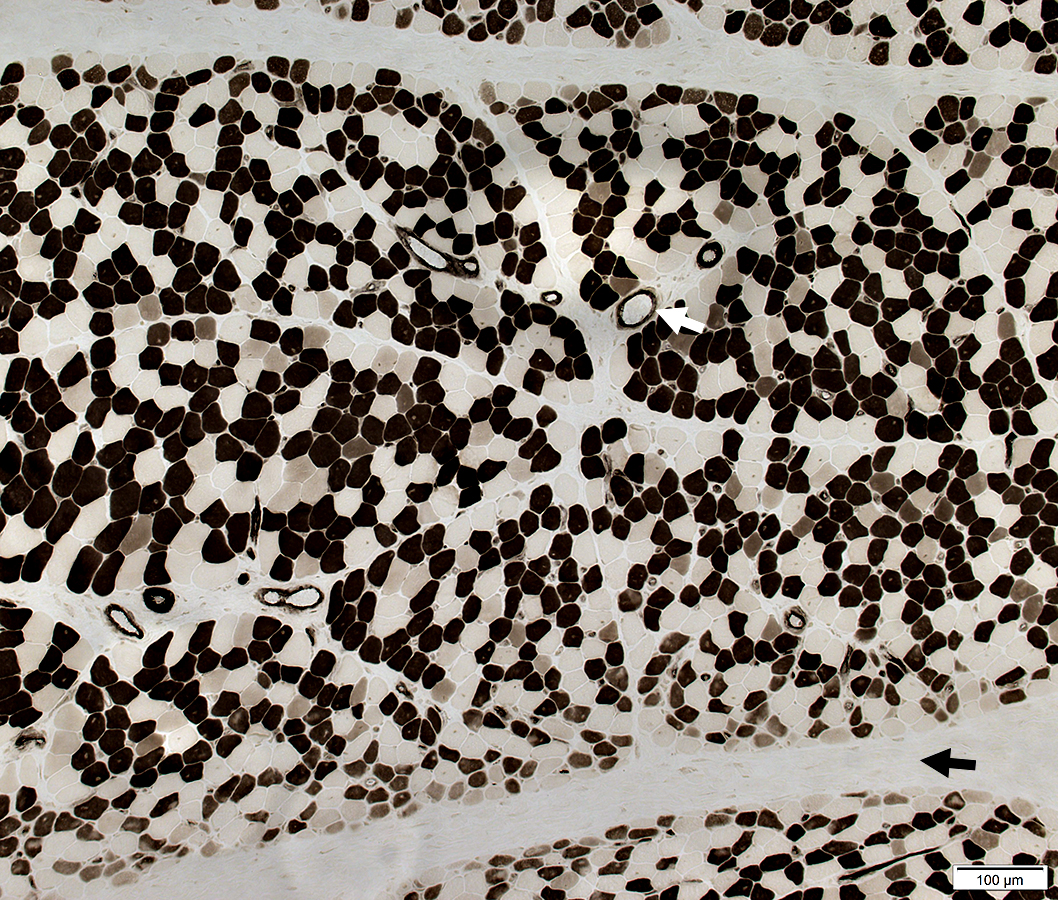 ATPase pH 4.3 stain |
Atrophic perifascicular muscle fibers neighbor long regions of avascular perimysium.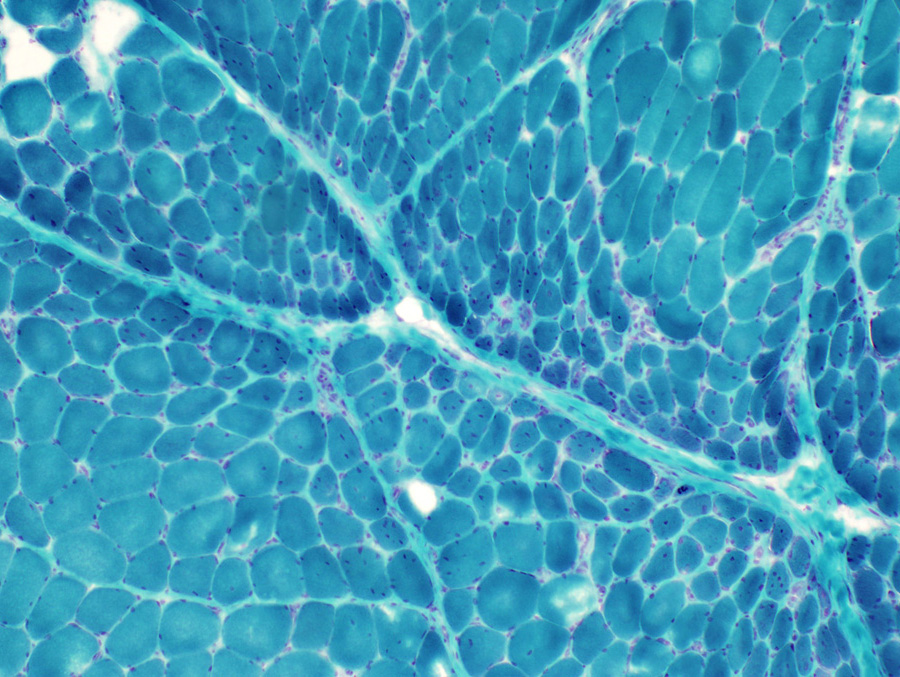 Gomori trichrome stain |
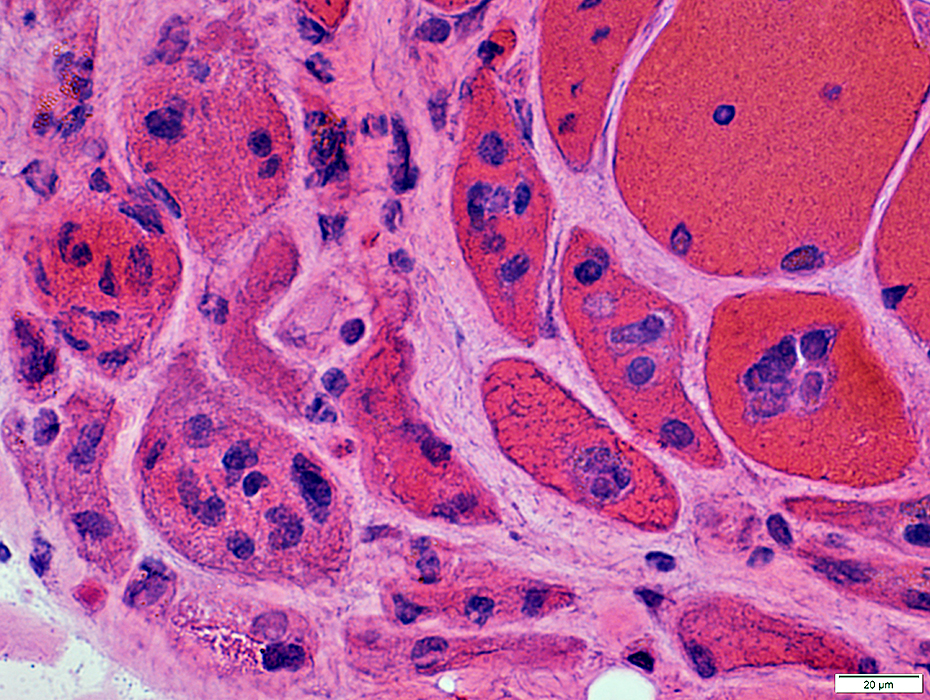
Atrophic perifascicular muscle fibers neighbor a long region of avascular perimysium.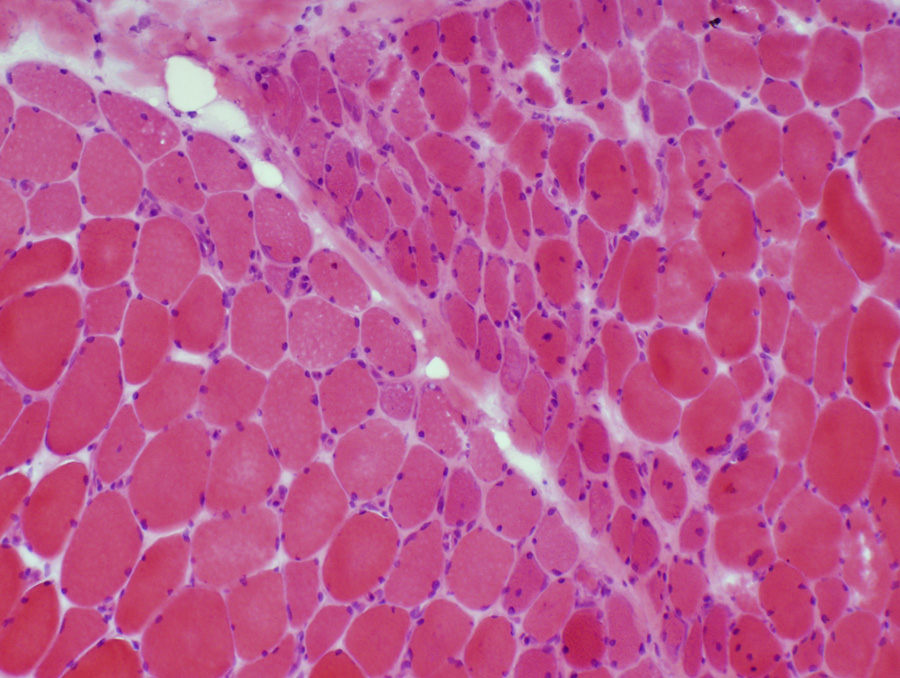 H&E stain Atrophic perifascicular muscle fibers have basophilic cytoplasm and large nuclei. Some perifascicular muscle fibers have basophilic or eosinophilic aggregates 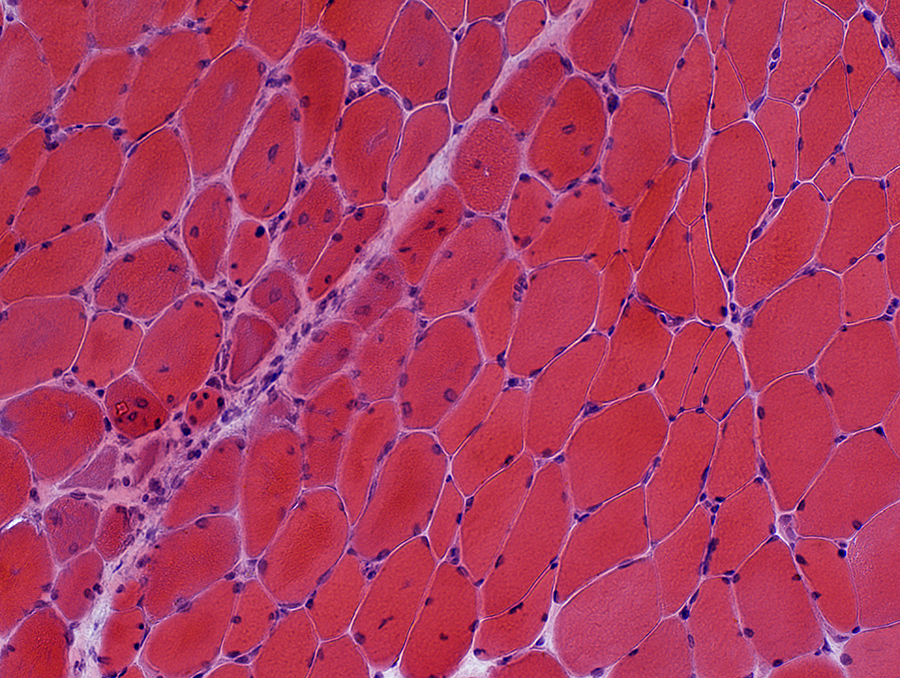 H&E stain Perifascicular muscle fiber pathology: Cytoplasmic aggregates (dark staining) & Internal nuclei. 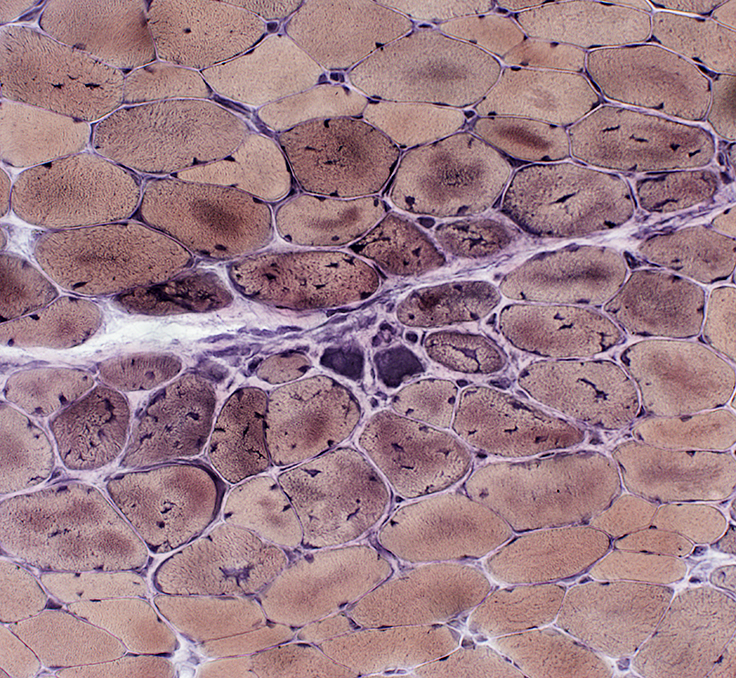 VvG stain |
Perifascicular pathology: Other stains
NADH
 NADH stain Muscle fibers near avascular perimysium: Small & Stain darkly Muscle fibers near vascular perimysium: More normal (Below, Arrow) 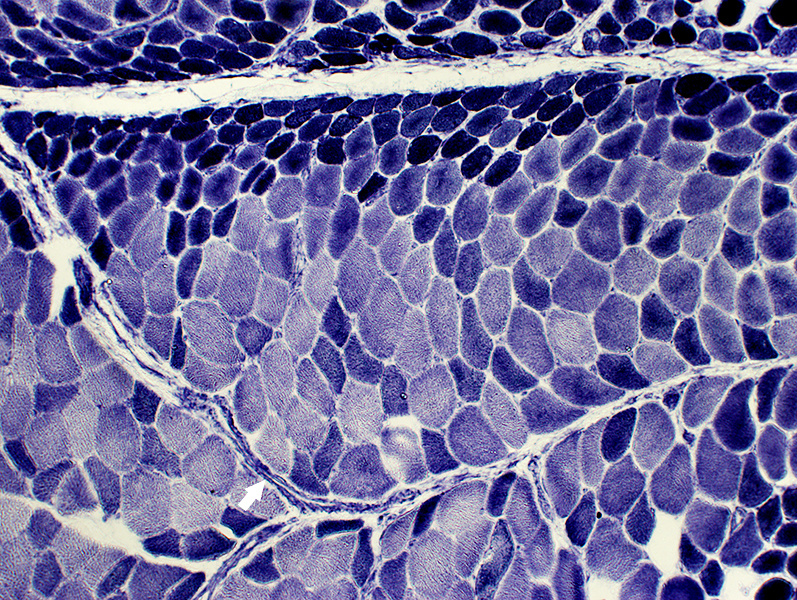 NADH stain |
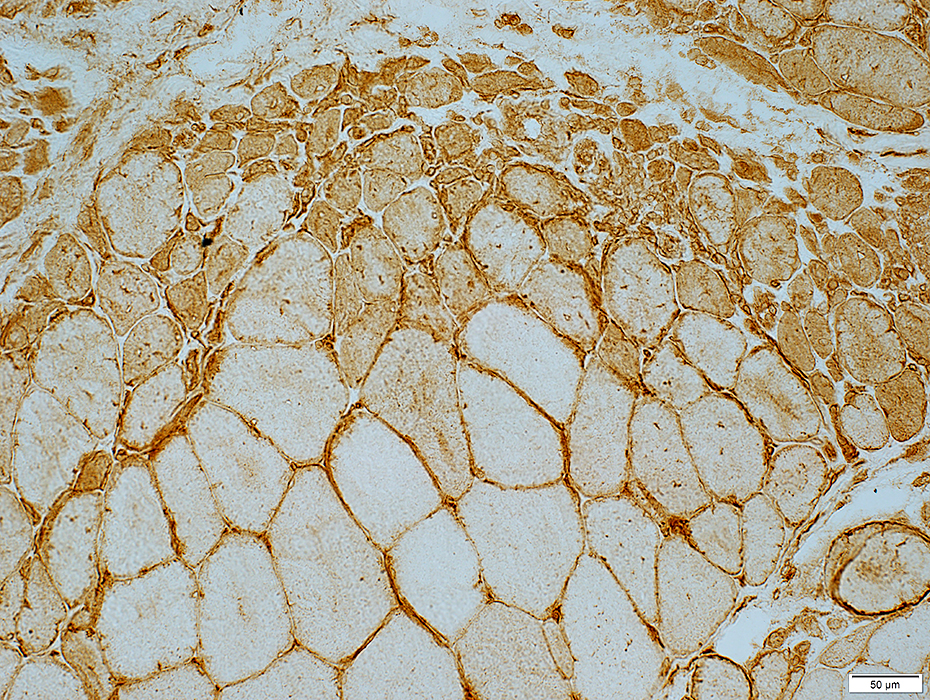
MHC Class I
Upregulated at edges of fascicles near avascular perimysium.
Less, or no, staining, near perimysium containing larger vessels (Arrows)
 MHC Class I stain |
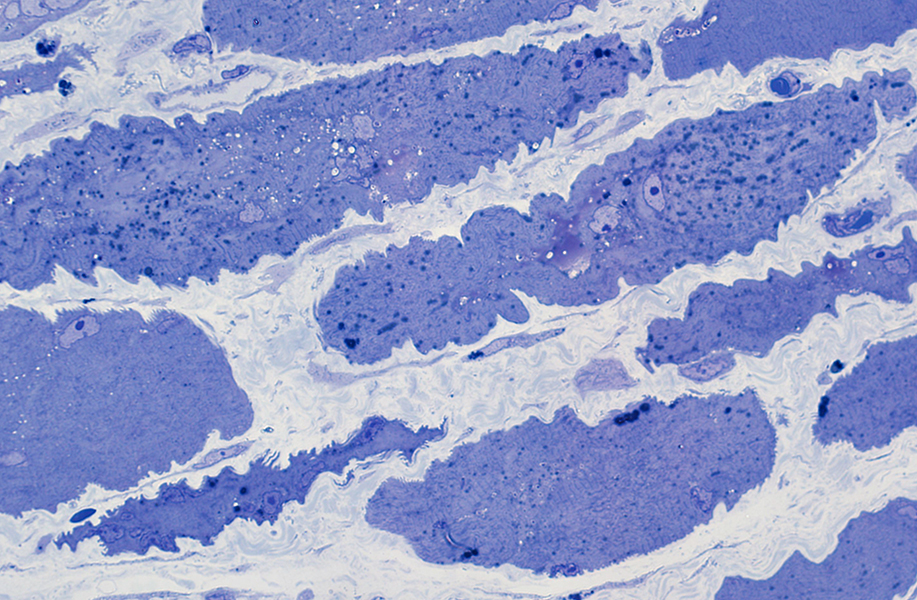
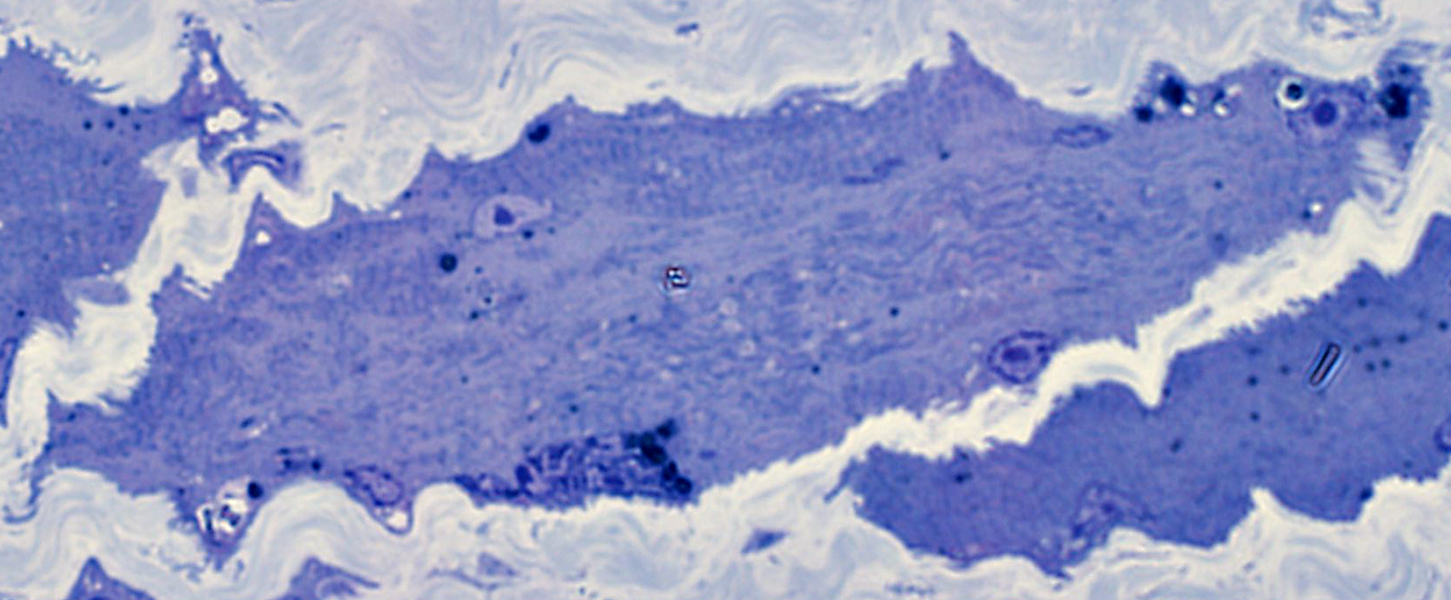
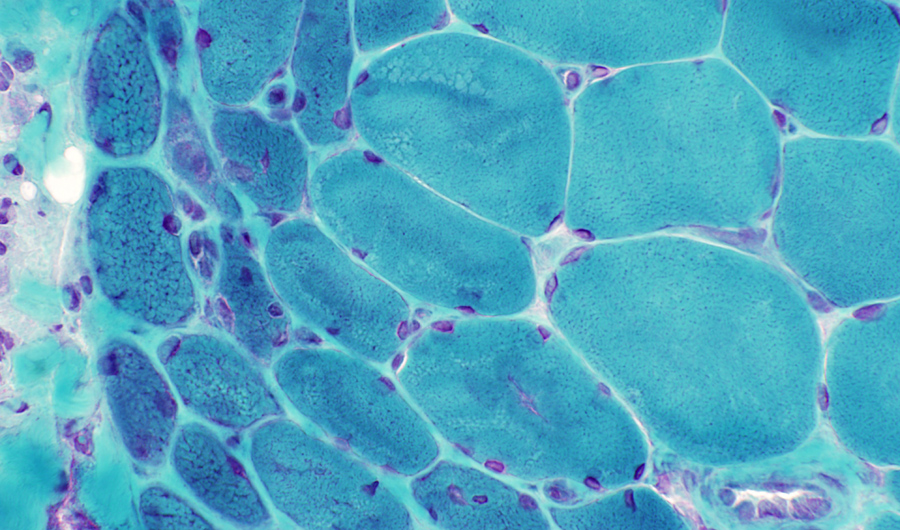
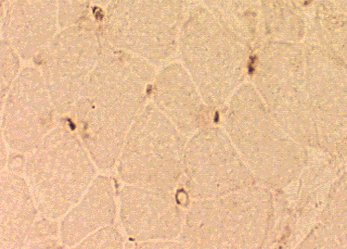
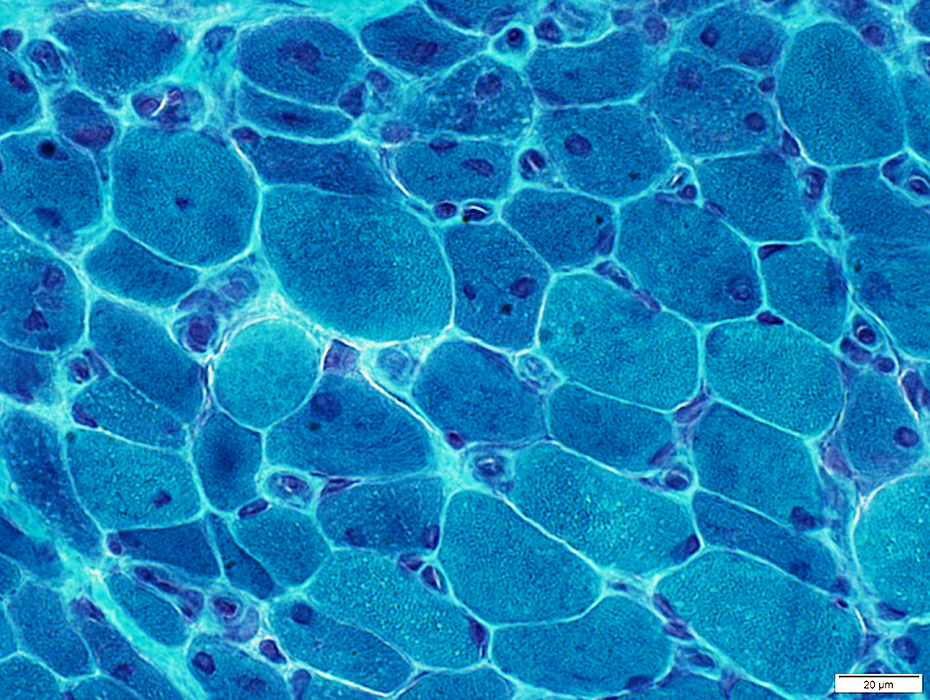
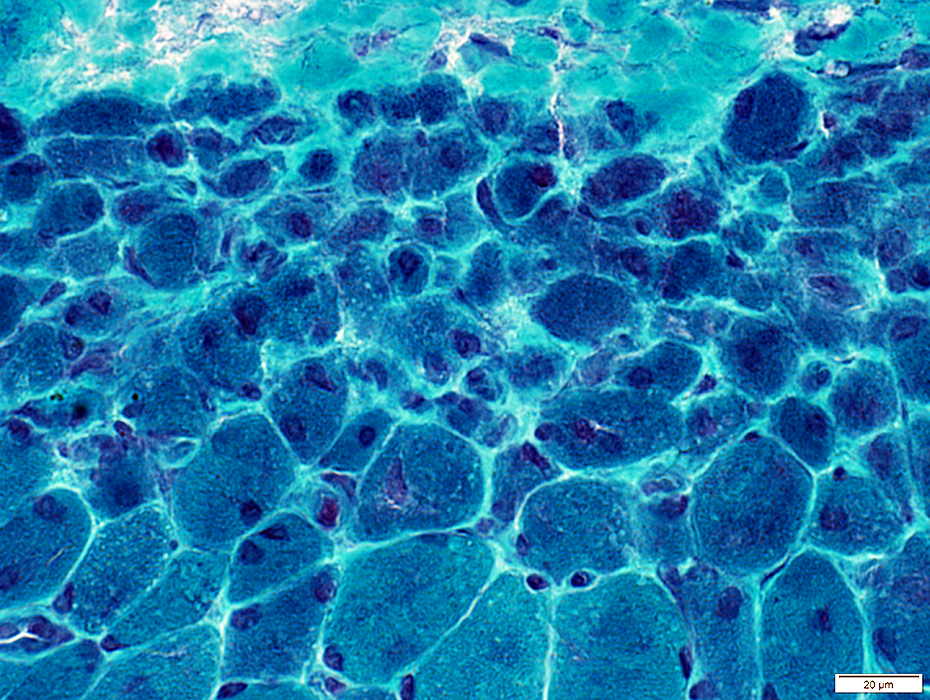
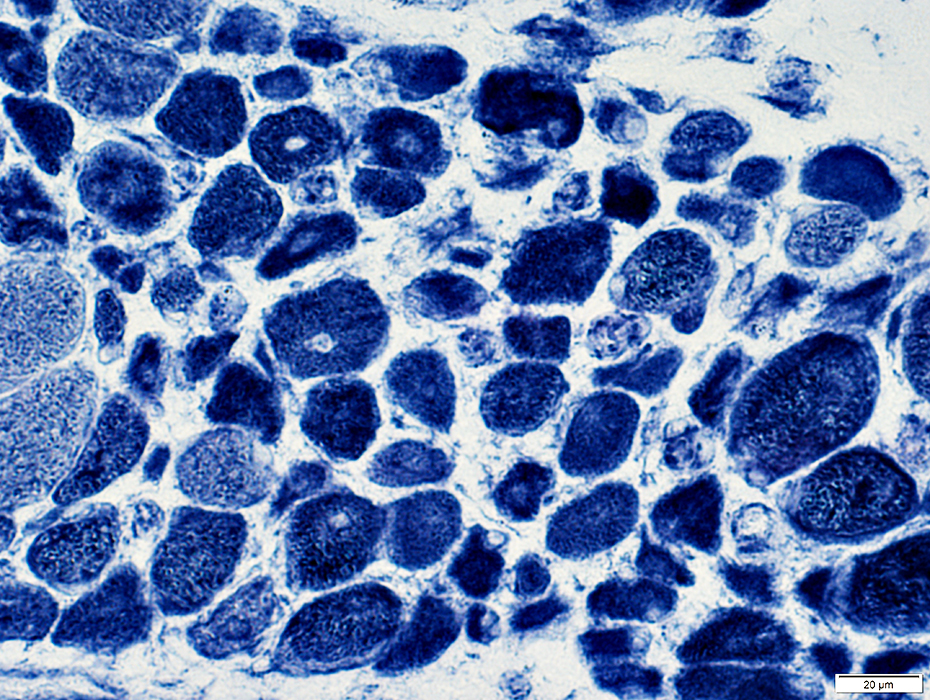
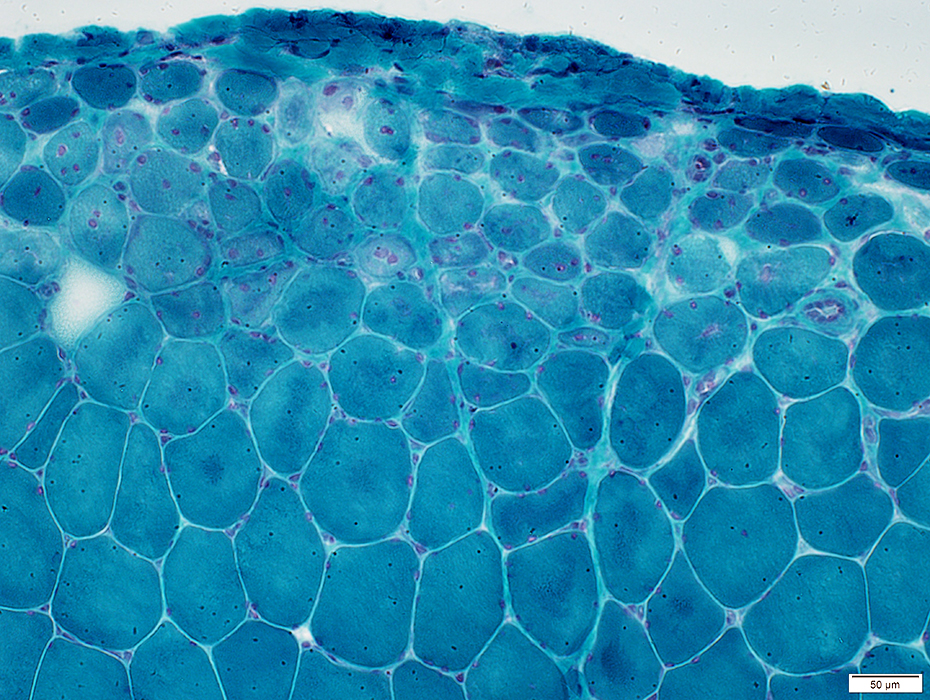
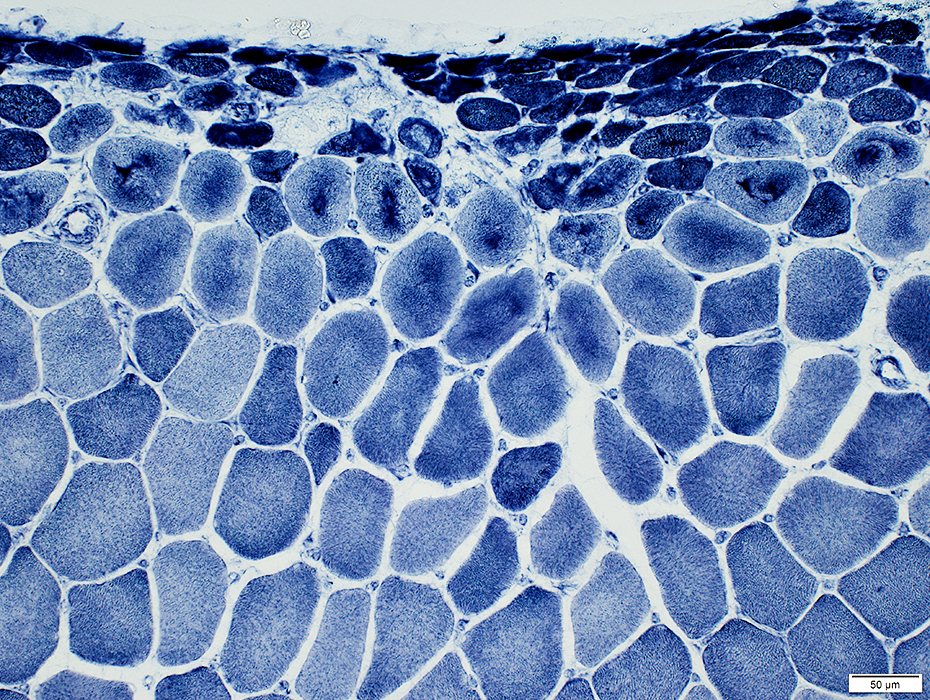
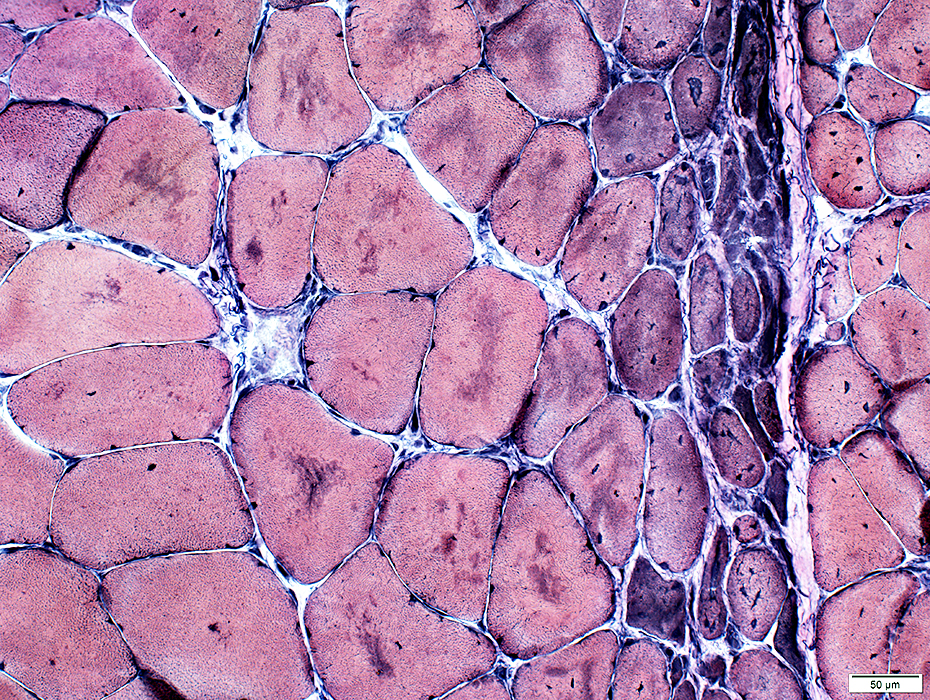
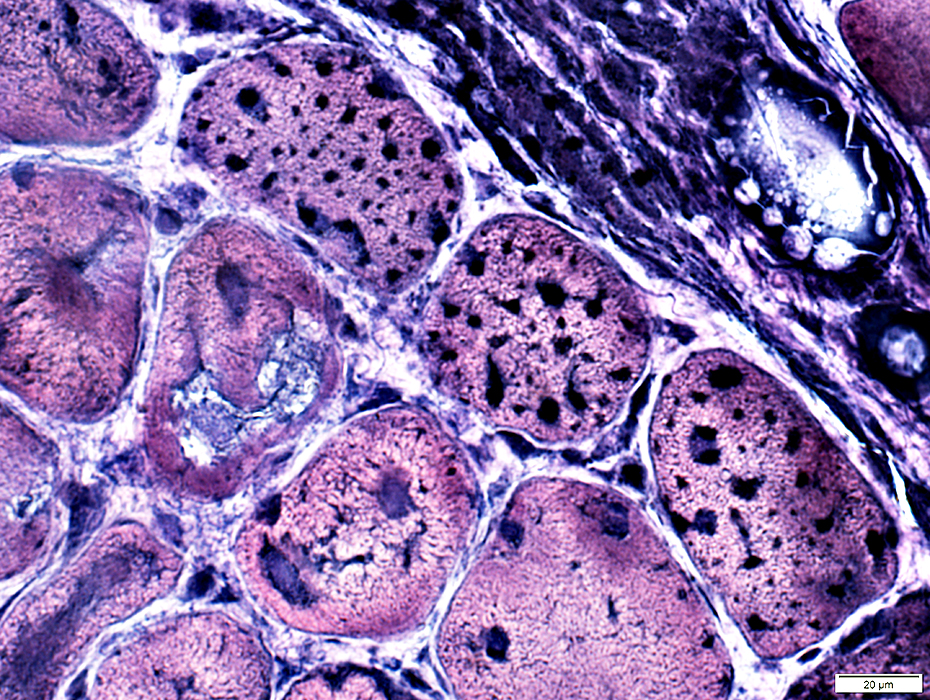
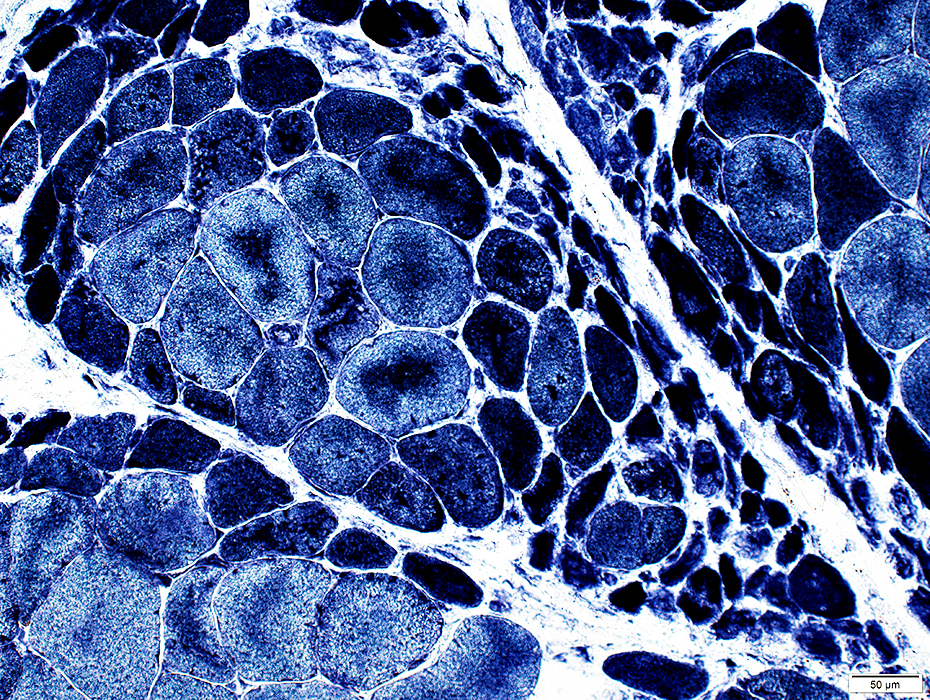
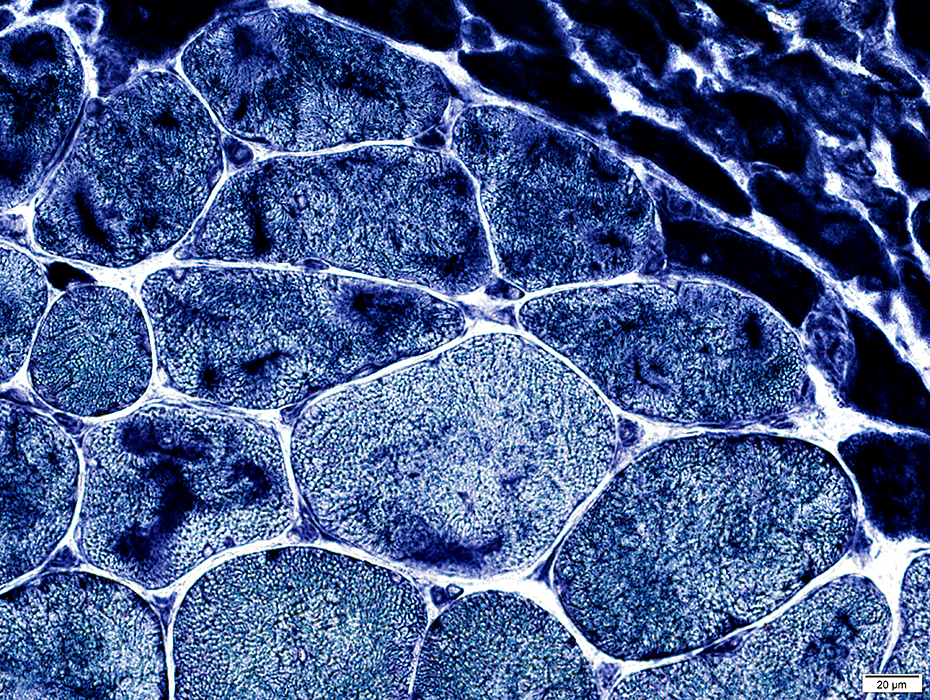
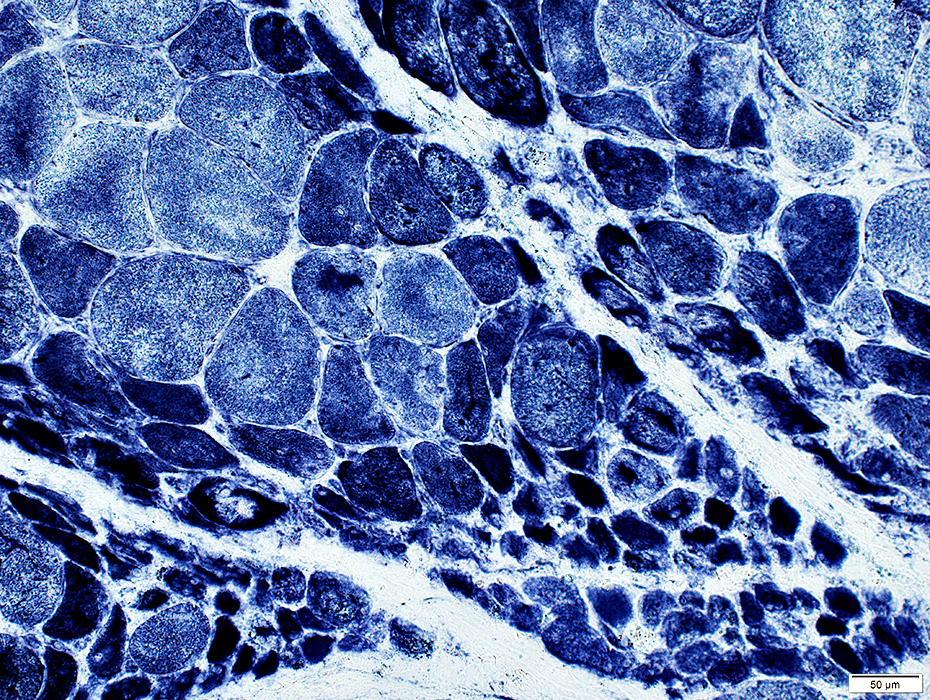
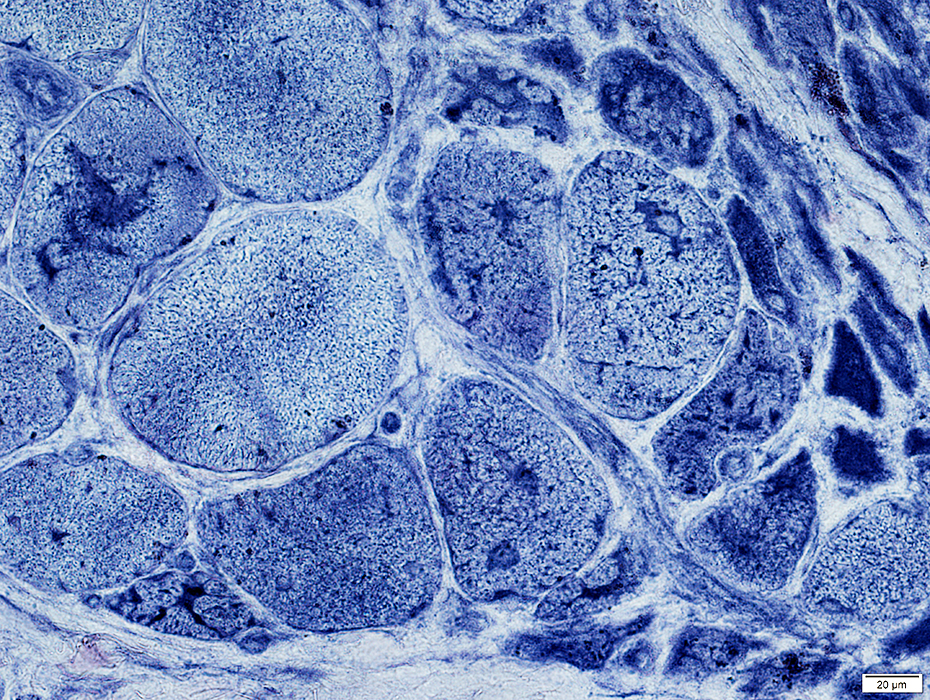
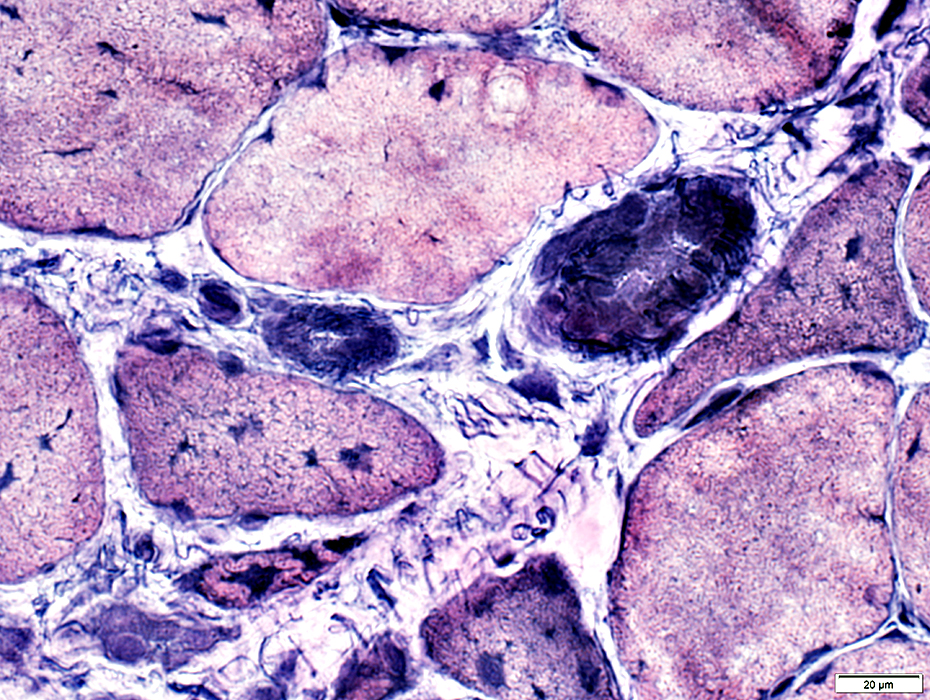
Perifascicular atrophy: Toluidine blue-stained plastic sections
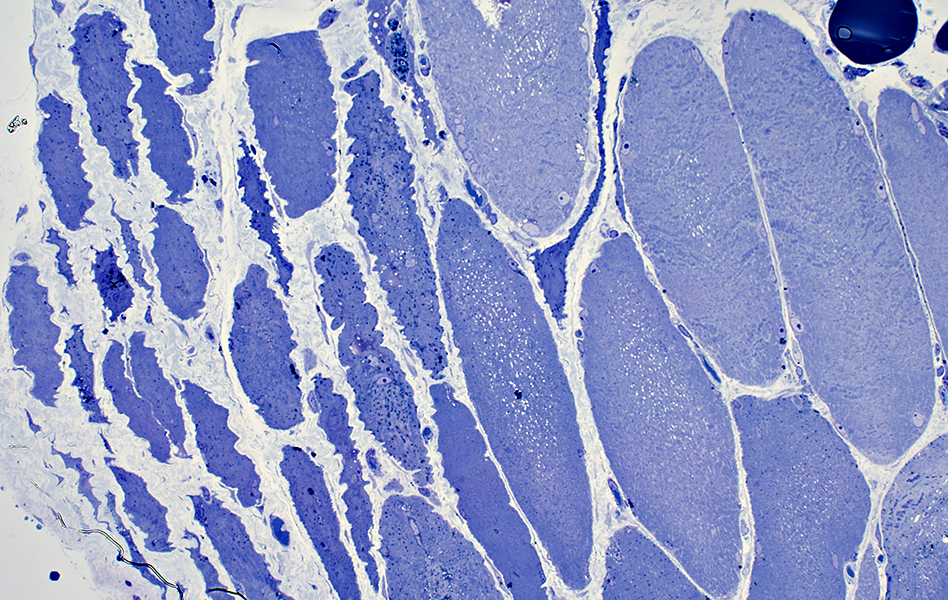
|
|
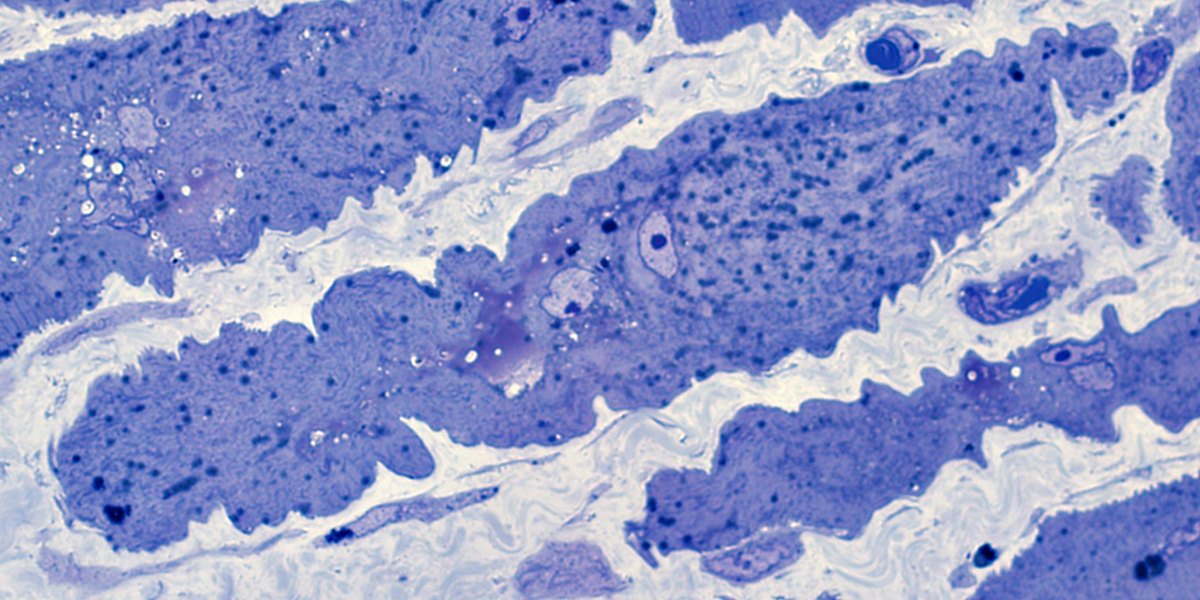
|
Size: Atrophic
Sarcolemmal membrane: Irregular
Contain lipid droplets
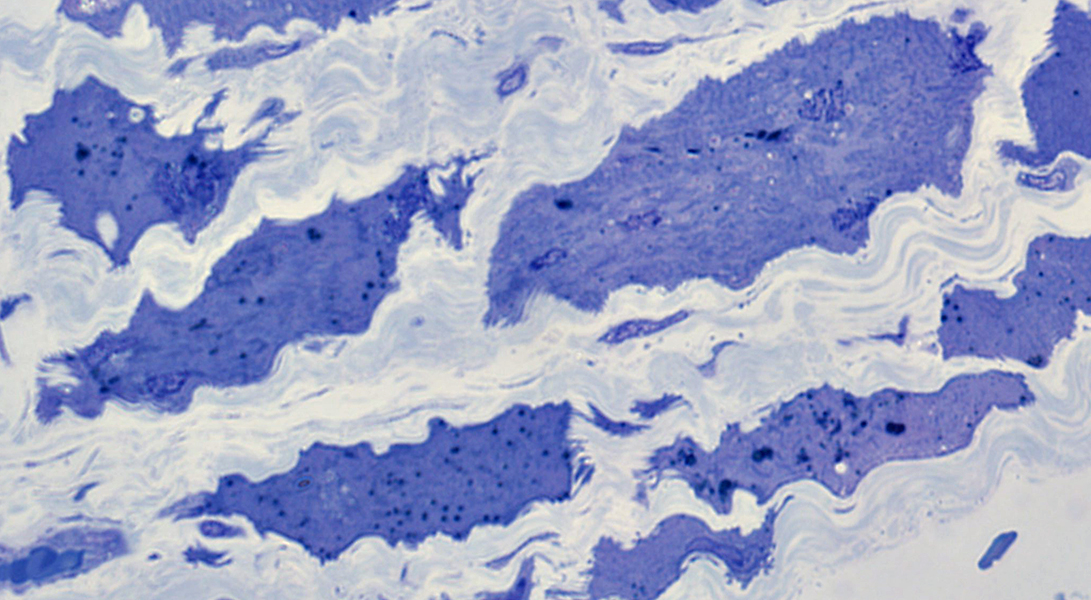
|
|
MITOCHONDRIAL PATHOLOGY
The extent of the perifascicular muscle fiber pathology in active DM is often more prominent on cytochrome oxidase stain.
SDH stain is not reduced.
Reduced cytochrome oxidase staining is not typically present in IMPP syndromes which have a different pattern of perifascicular muscle fiber pathology.
Cytochrome Oxidase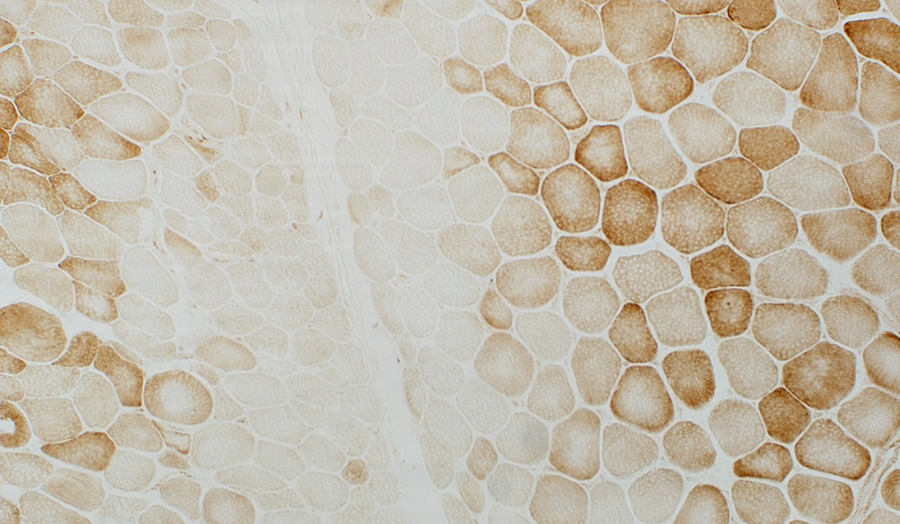 COX stain Muscle fibers near avascular perimysium are small & have pale COX staining Succinate Dehydrogenase 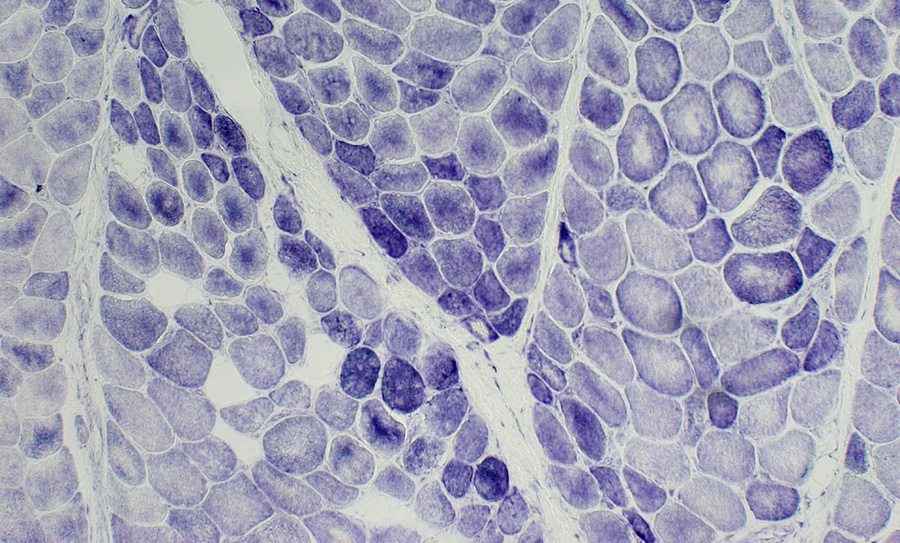 SDH stain Muscle fibers near the avascular perimysium are small & have normal or dark SDH staining |
Perifascicular muscle fibers near avascular perimysium: Small; Pale COX staining, Blue (SDH) color
 COX + SDH stain |
Mildy reduced COX stain in perifascicular muscle fibers with normal size. (Arrow; Right)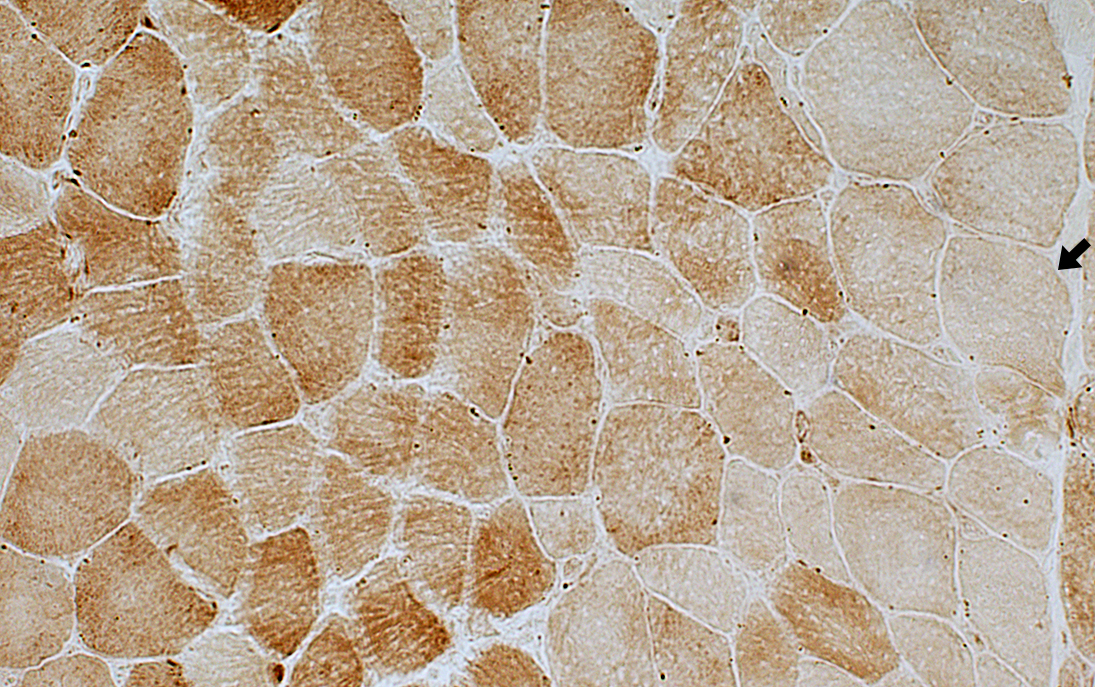 COX stain |
|
Perifascicular atrophy: ATPase pH 9.4 stain 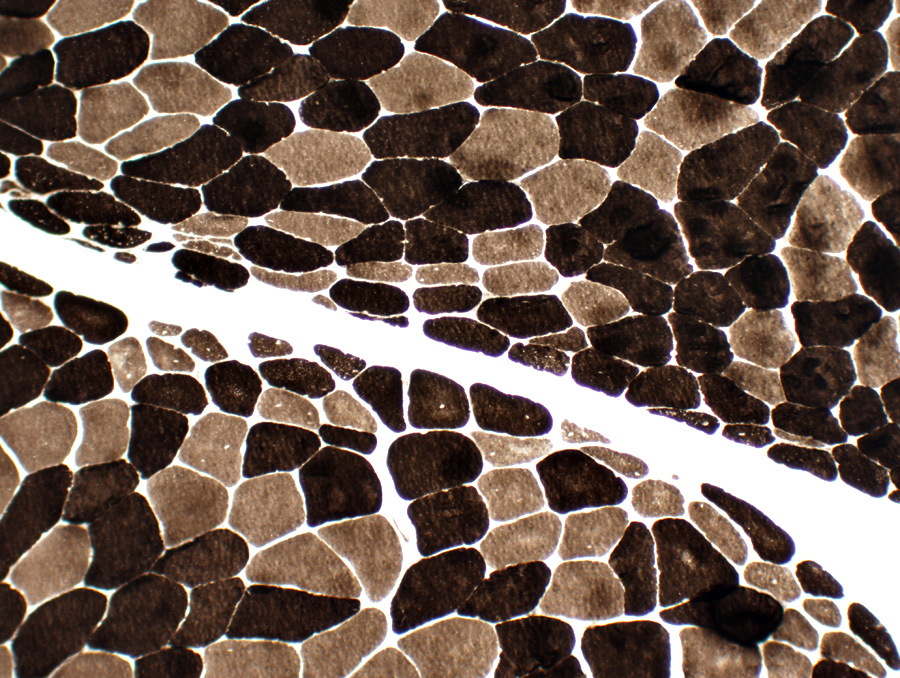 ATPase pH 9.4 stain Perifascicular atrophy is often especially obvious on ATPase stains. Small fibers: Both types I & II. |
ATPase pH 4.3
 ATPase pH 4.3 stain |
 ATPase pH 4.3 stain |
 ATPase pH 4.3 stain |
Type IIC muscle fibers (intermediate staining): Present in regions of atrophy & larger muscle fibers.
Type 1 muscle fibers: Few, or none, in regions of most severe atrophy at edge of fascicles (Above; Dark arrow).
Small muscle fibers: Located near avascular perimysium.
Fibers near intermediate-sized perimysial vessel (Below; White arrow): Larger size.
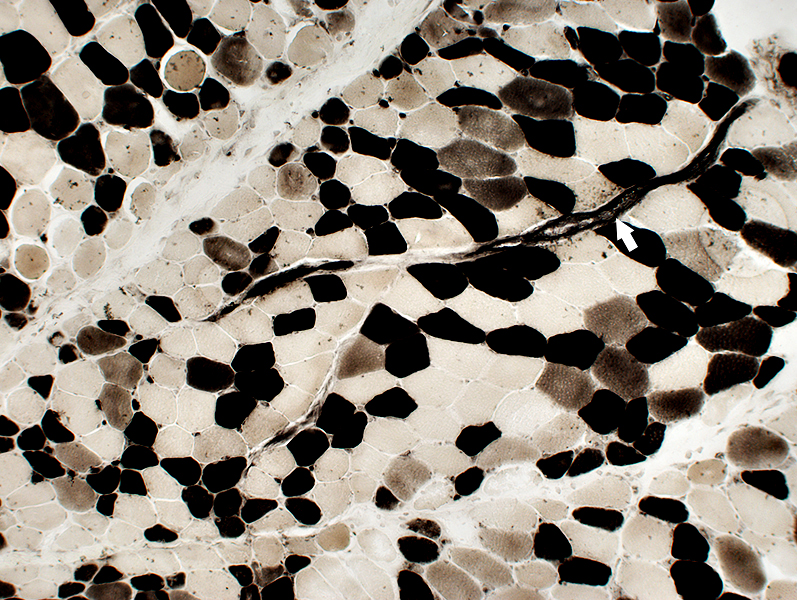 ATPase pH 4.3 stain |
PAS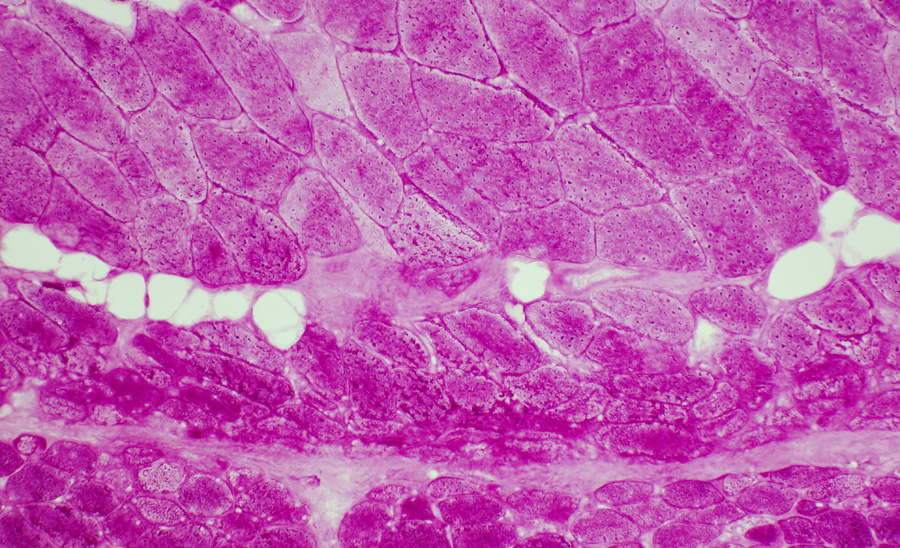 PAS stain DM-VP: Increased glycogen staining in small perifascicular muscle fibers.1 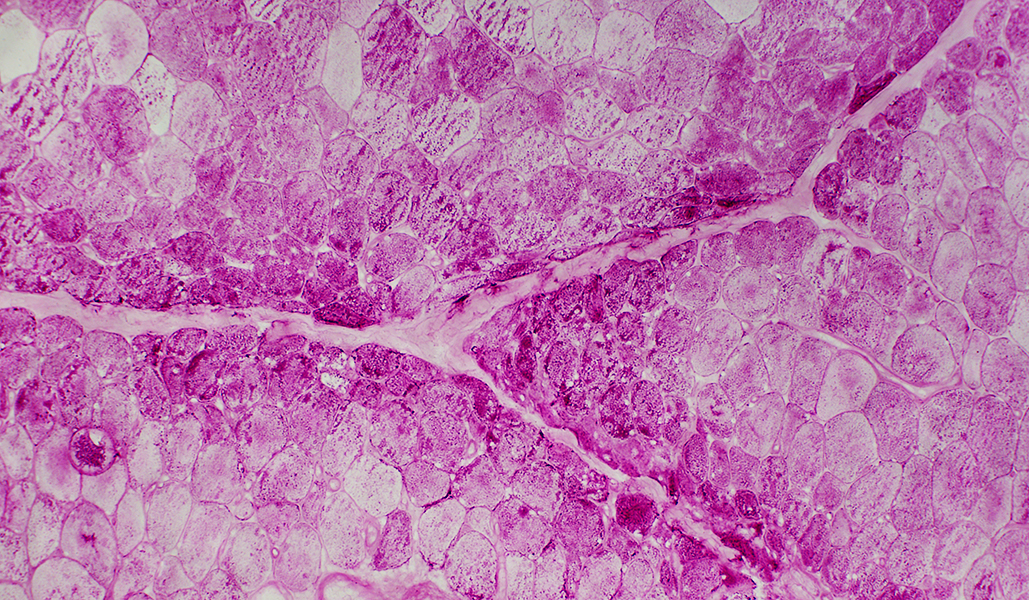
|
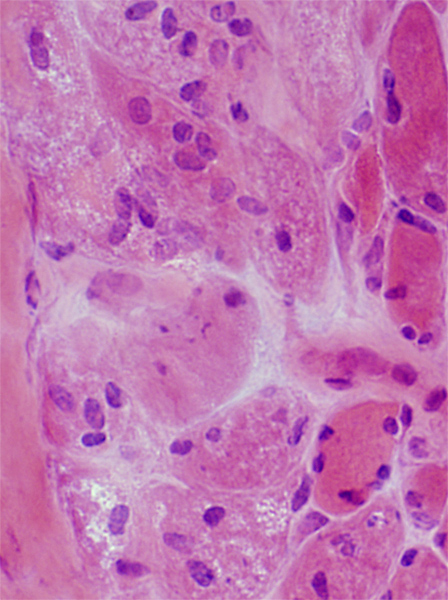
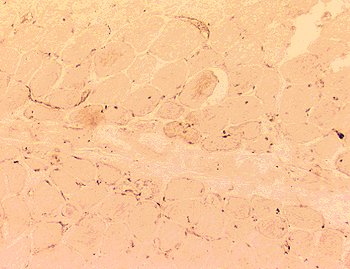
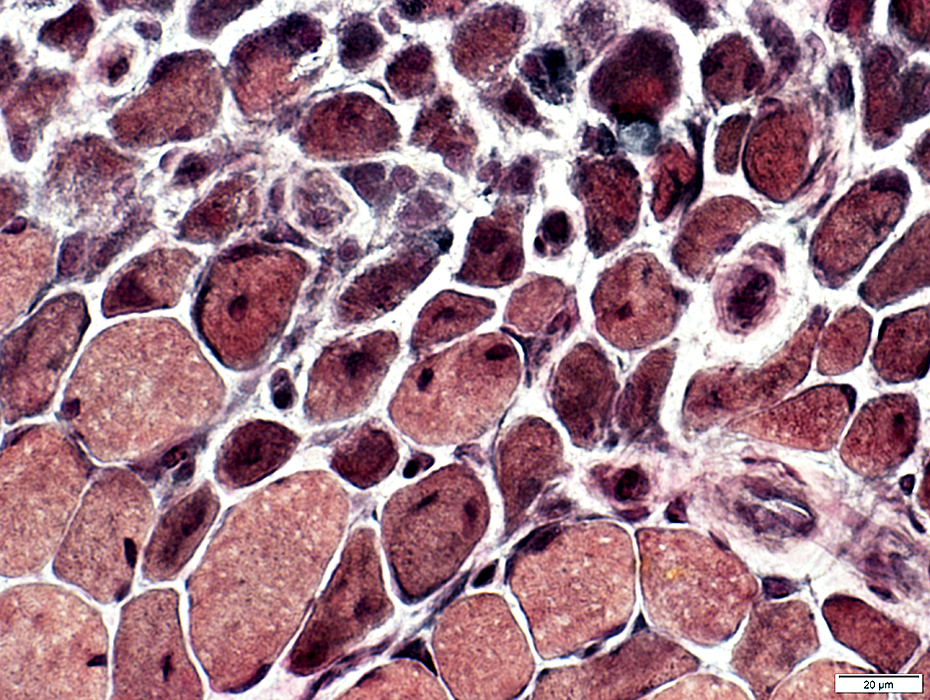
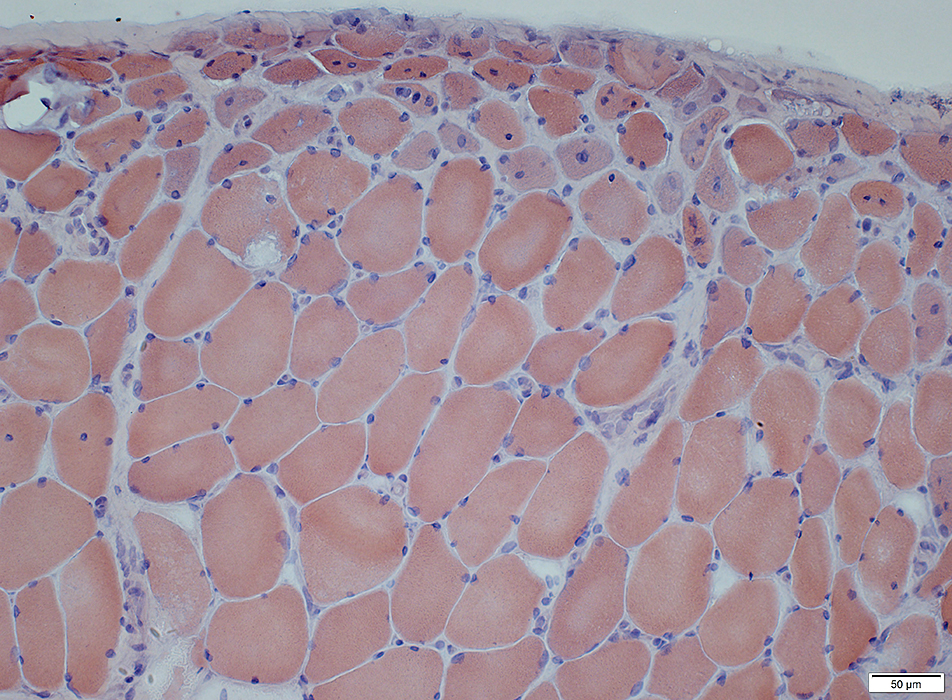
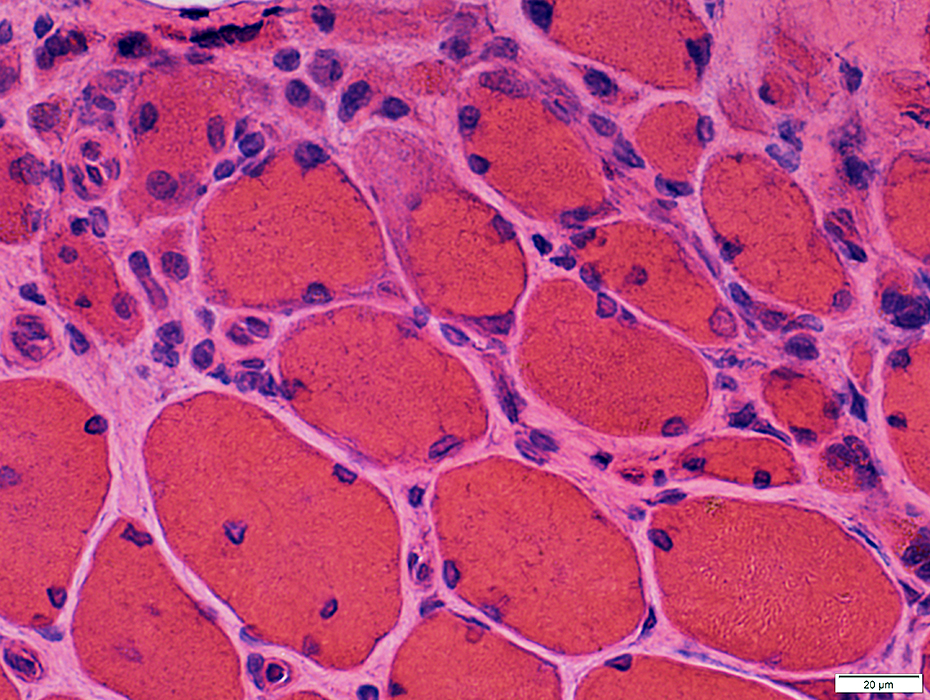
Perifascicular muscle fiber atrophy: Fiber pathology
Muscle fibers in regions of perifascicular pathology show several abnormalities in addition to being small.Some muscle fibers have
Vacuolar or reticulated cytoplasm (Below).
Cytochrome oxidase staining reduced
MHC-I upregulation
Aggregates: LC3 & Caveolin-3
Muscle fiber nuclei are enlarged.
Muscle fiber necrosis is rare.
 H&E stain |
 GT stain |
 Congo red stain |
|
Muscle fibers may also have Coarse internal architecture with basophilia (Left, Arrow), or Internal nuclei (Right). The abnormal internal architecture may be better visualized on Gomori trichrome 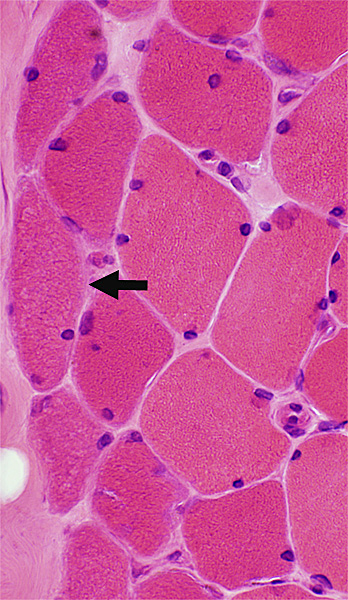
 H&E stain |
Abnormal internal architecture in dermatomyositis muscle fibers is more apparent on Gomori trichrome stains.
The abnormalities may be present in both small and large muscle fibers.
Cytoplasmic bodies may occur
  |
Cytoplasmic bodies
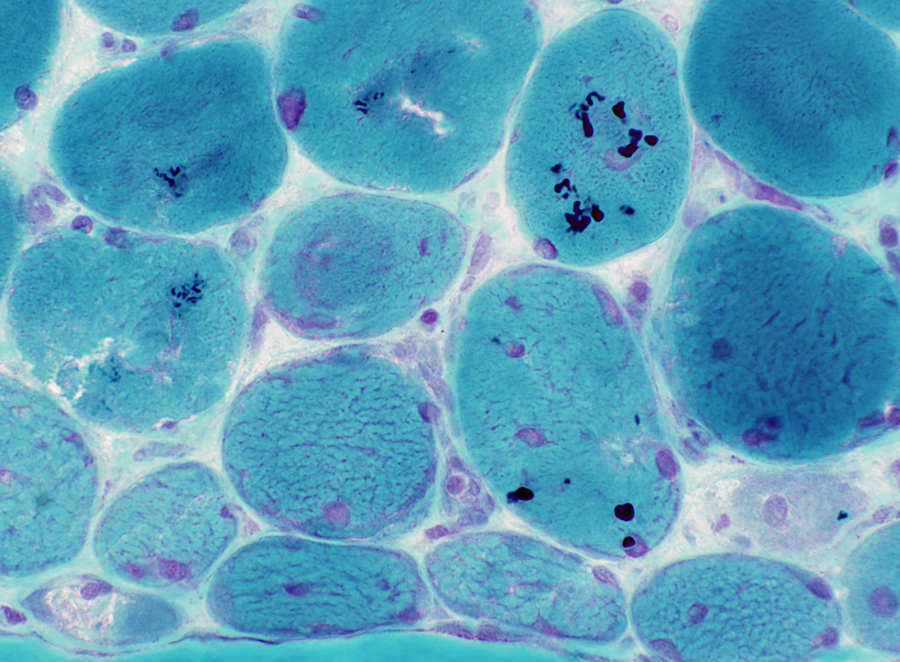 GT stain |
|
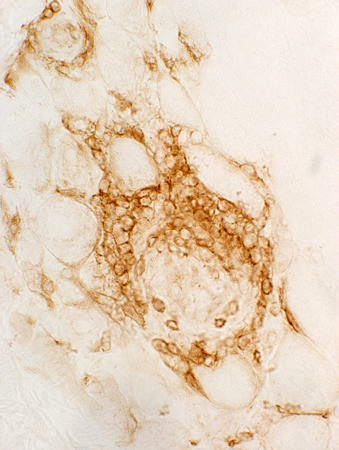
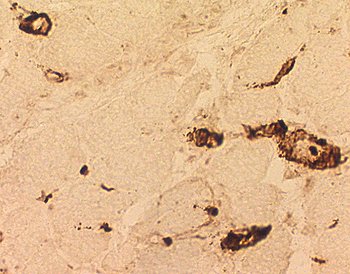
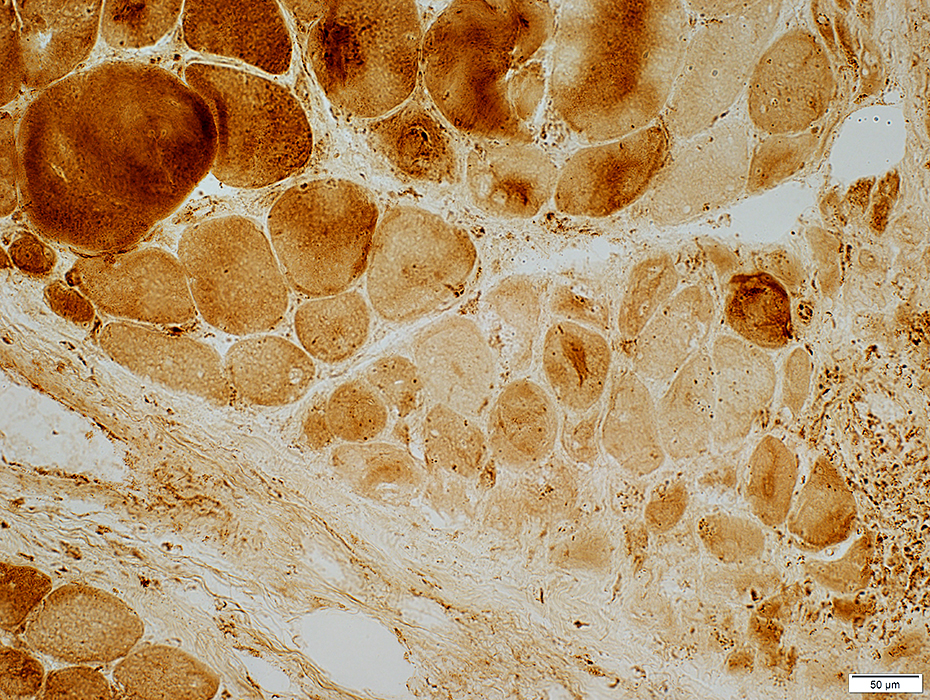
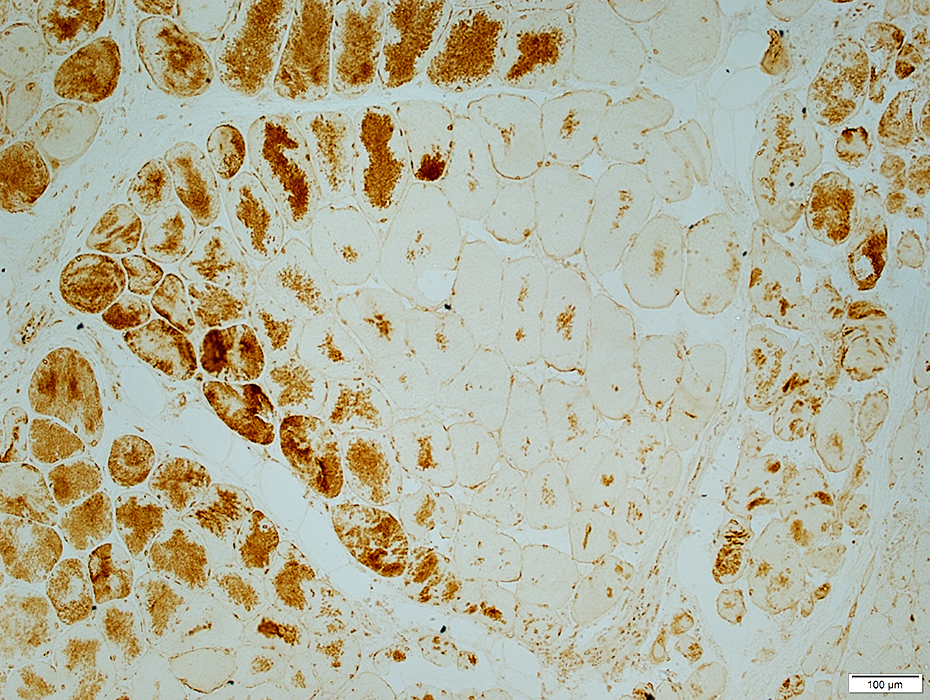
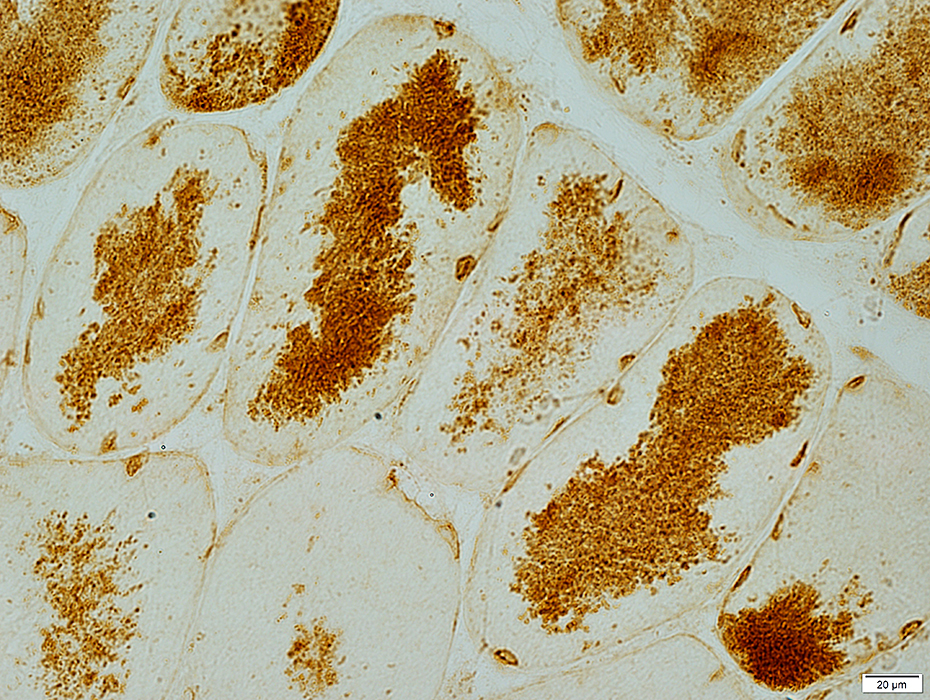
Aggregates: LC-3 & Caveolin-3 Aggregates and increased cytoplasmic staining are common in perifascicular muscle fibers with abnormal internal architecture in DM-VP. 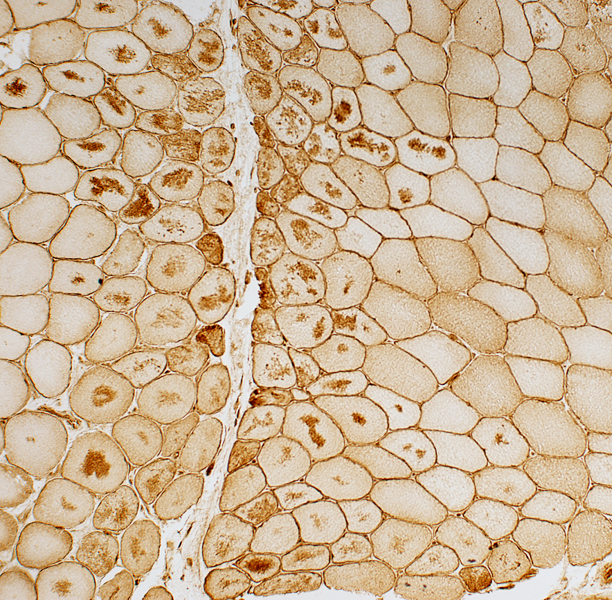
 Caveolin-3 stain |
 LC3 stain |
LC-3 aggregates: More prominent in muscle fibers toward edge of fascicle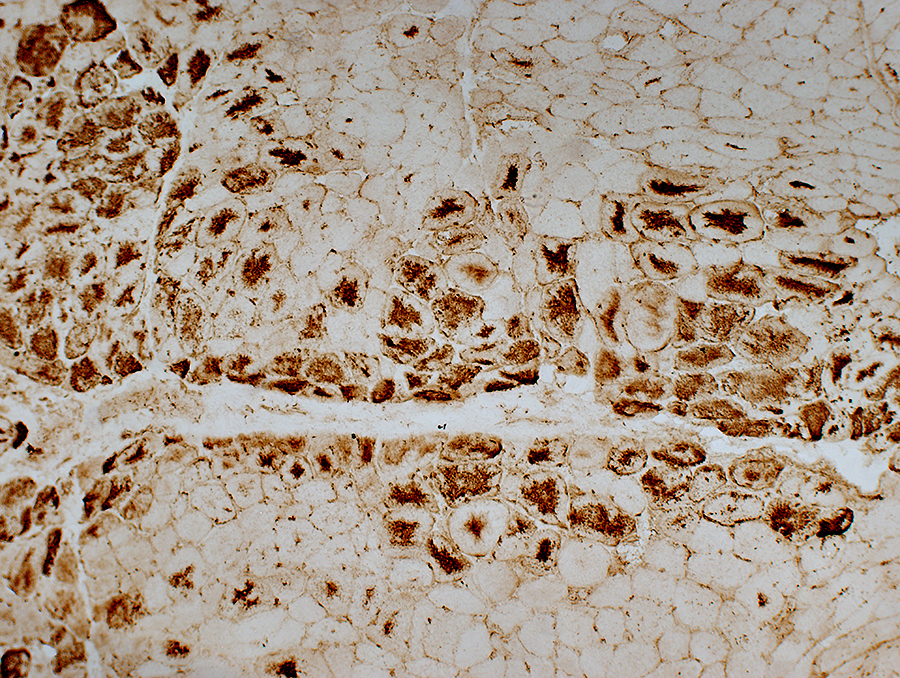
|
|
LC-3 aggregates: Irregular shaped in muscle fiber cytoplasm 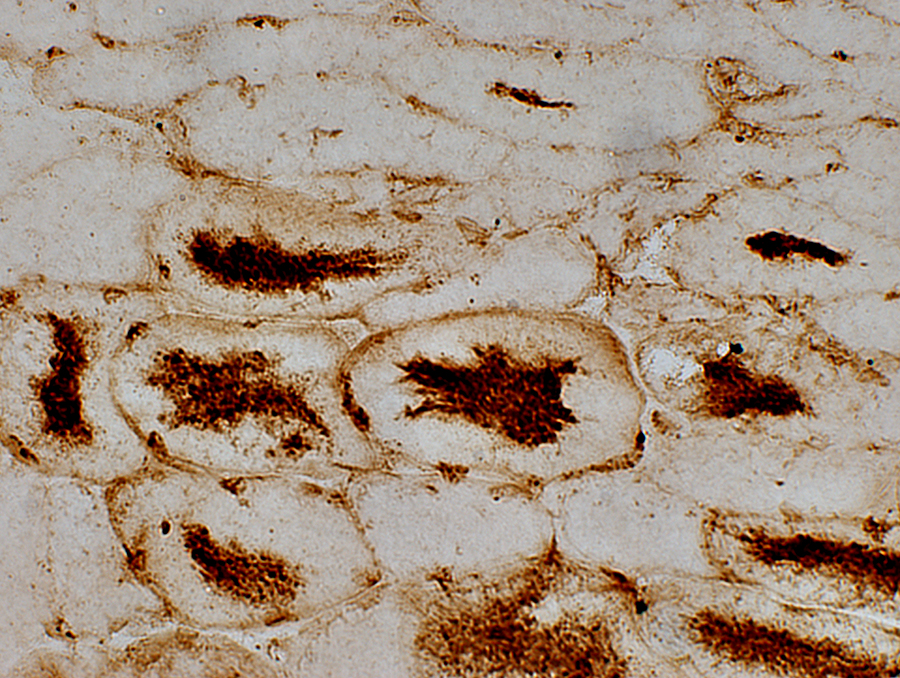
|
 AMPDA stain Aggregates in the center of muscle fibers |
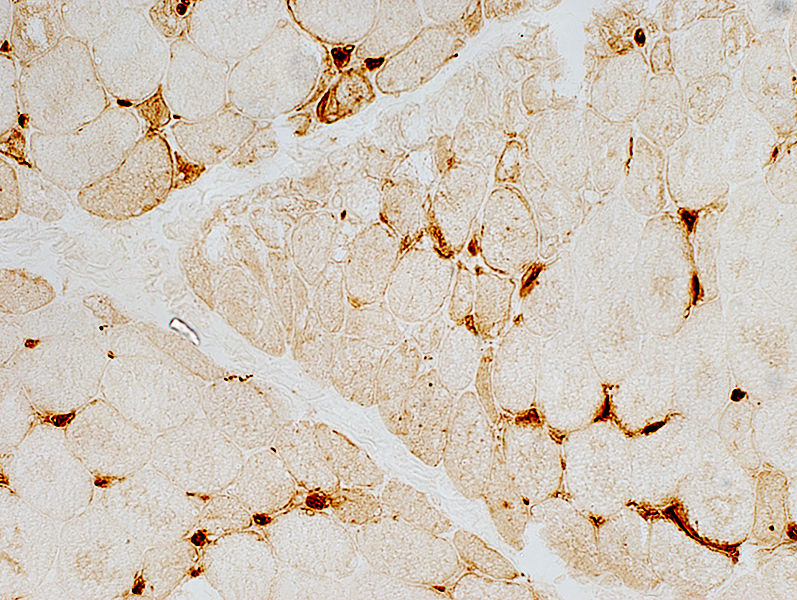
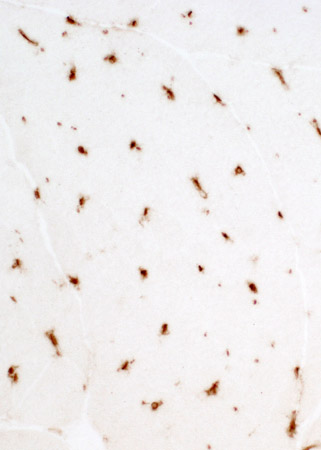
Dermatomyositis (DM-VP): MxA staining
|
DM-VP MxA strongly stains Perifascicular muscle fibers Endomysial capillaries 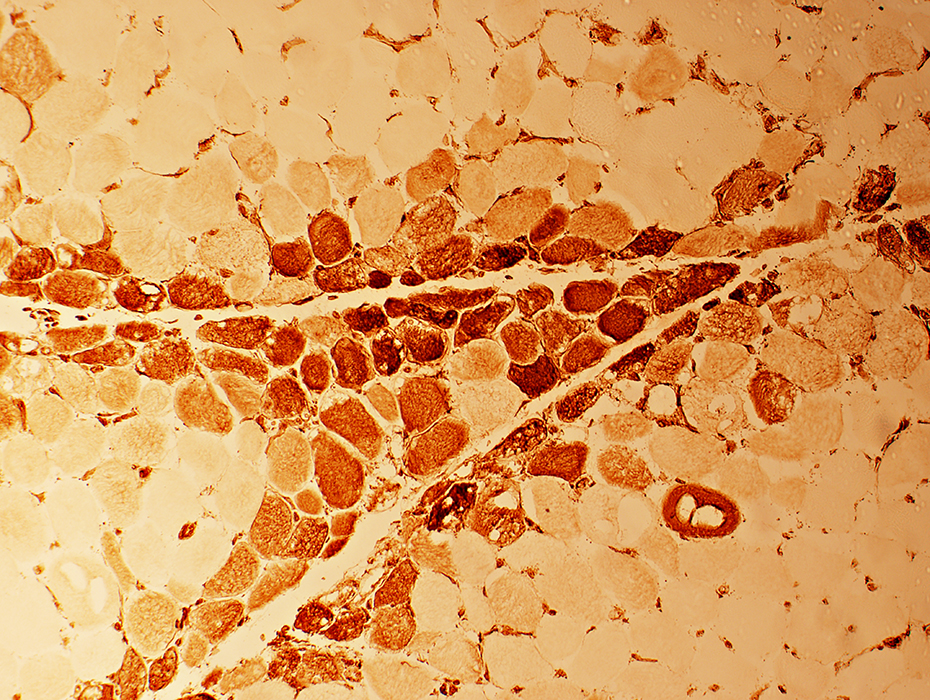 MxA stain |
|
Control Muscle No MxA staining of: Muscle fibers or Endomysial capillaries  MxA stain |
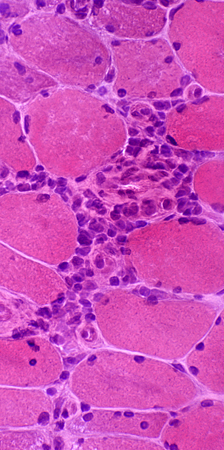
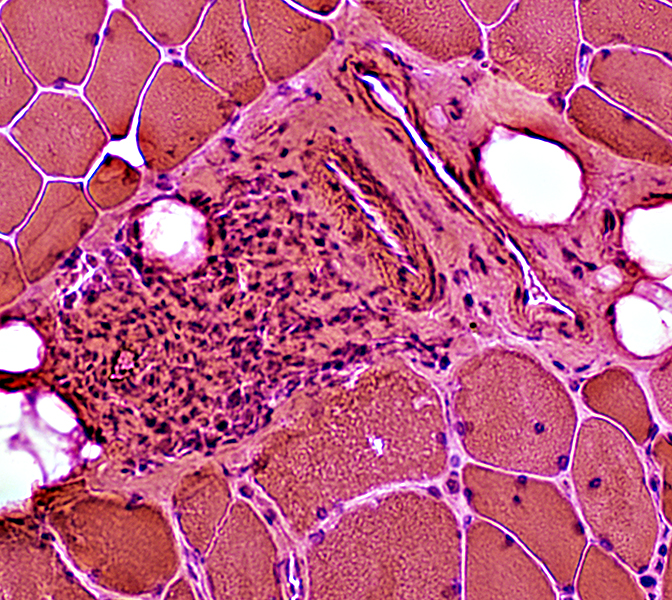
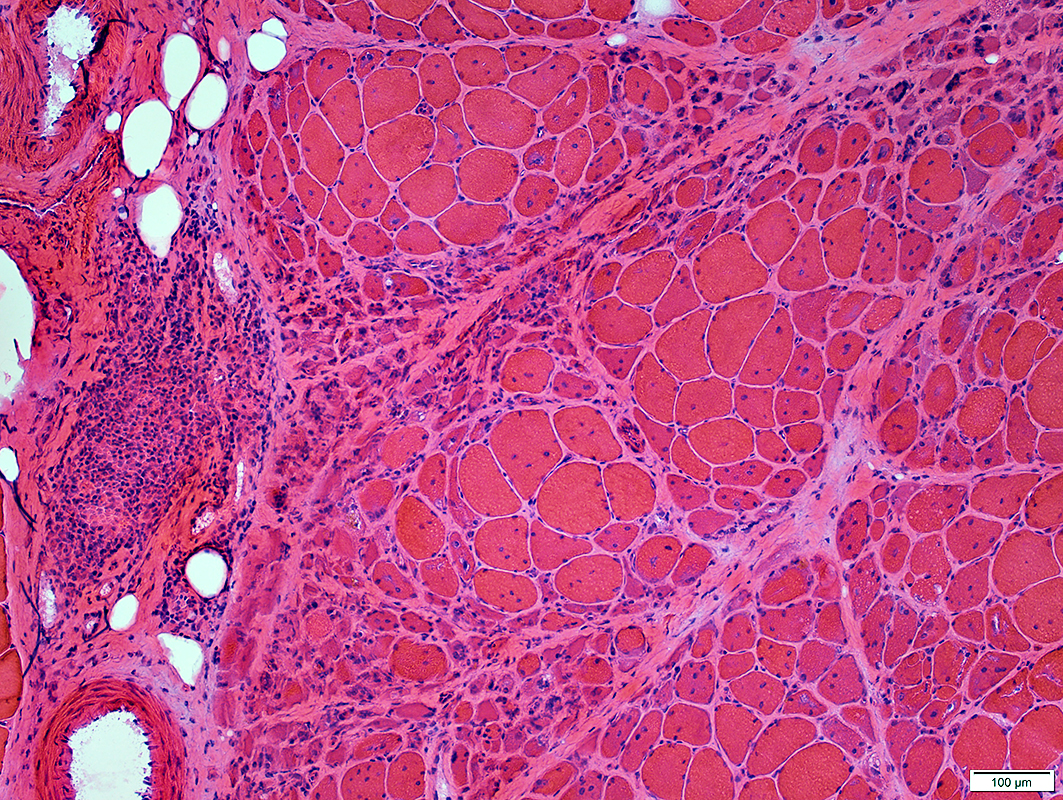
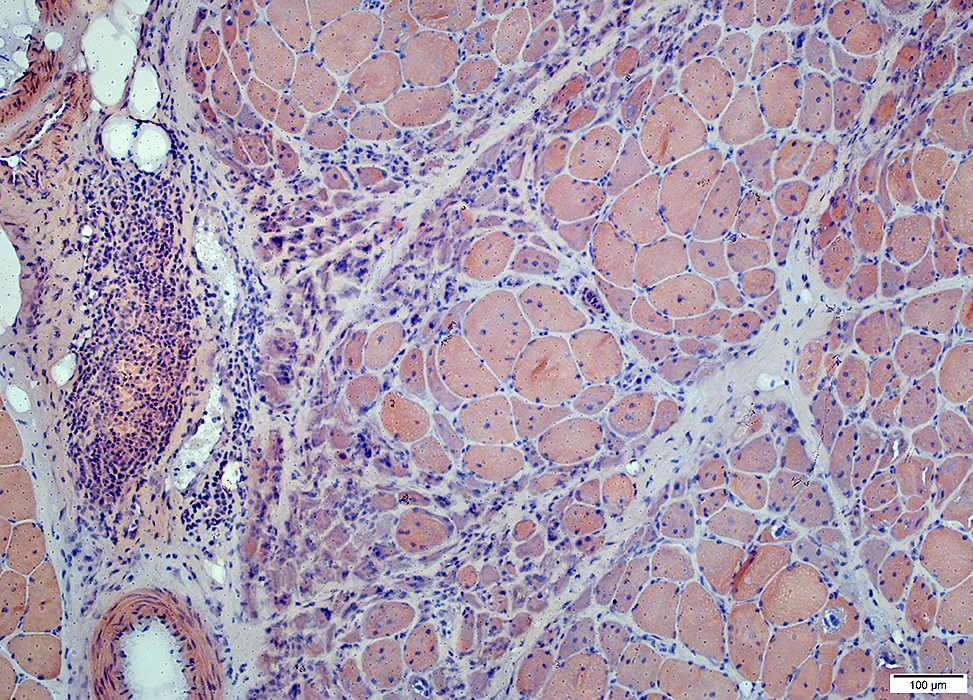
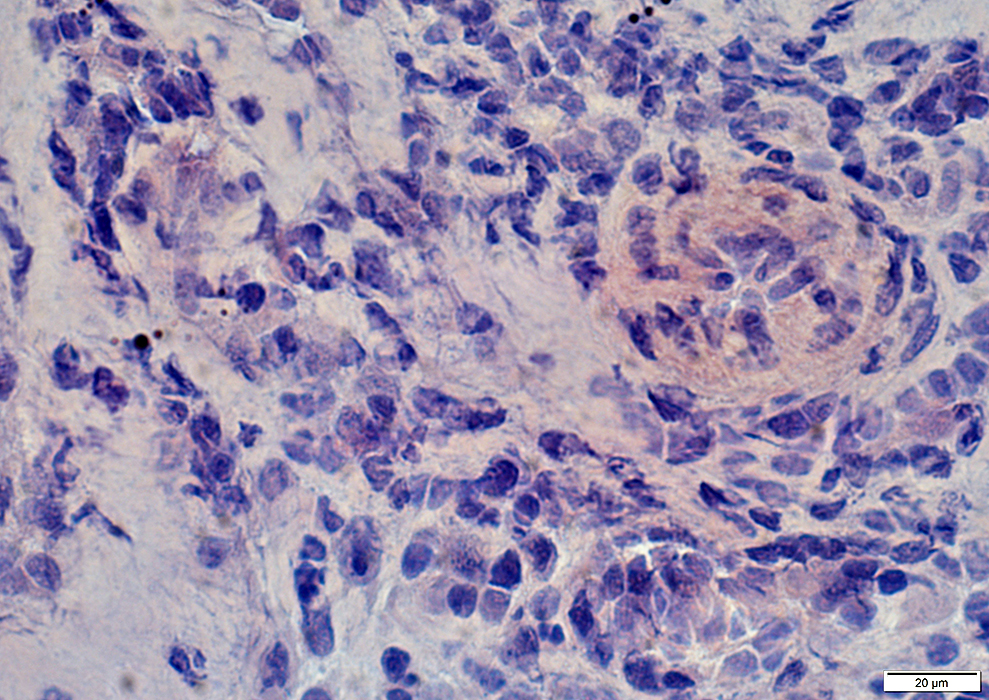
Dermatomyositis (DM-VP): Inflammation
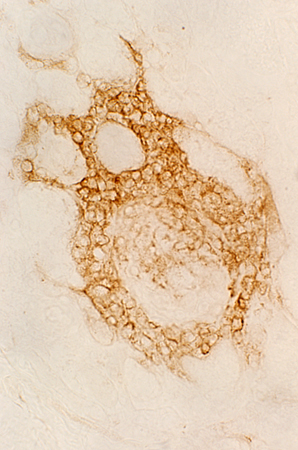
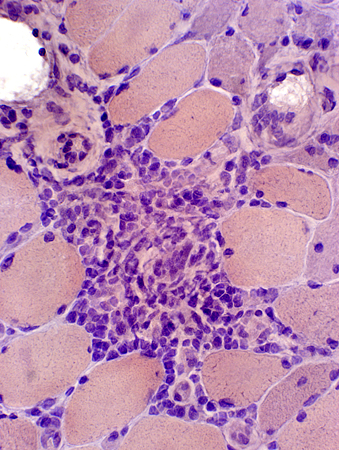
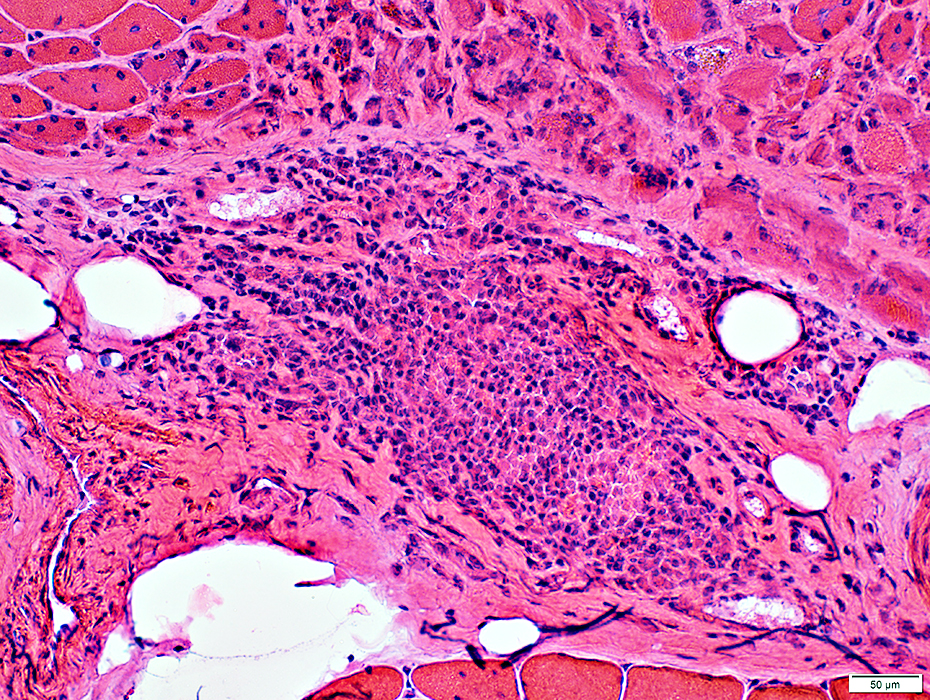
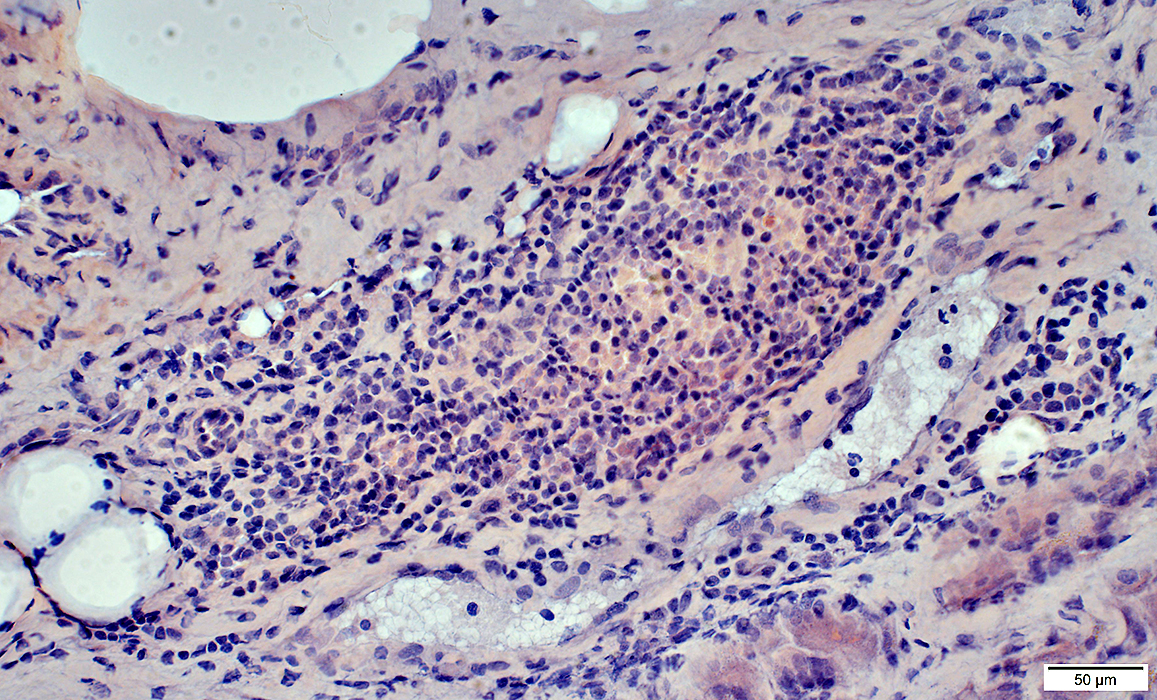
DM-VP: Mononuclear cell focus
Location: Separate from atrophic perifascicular muscle fibers
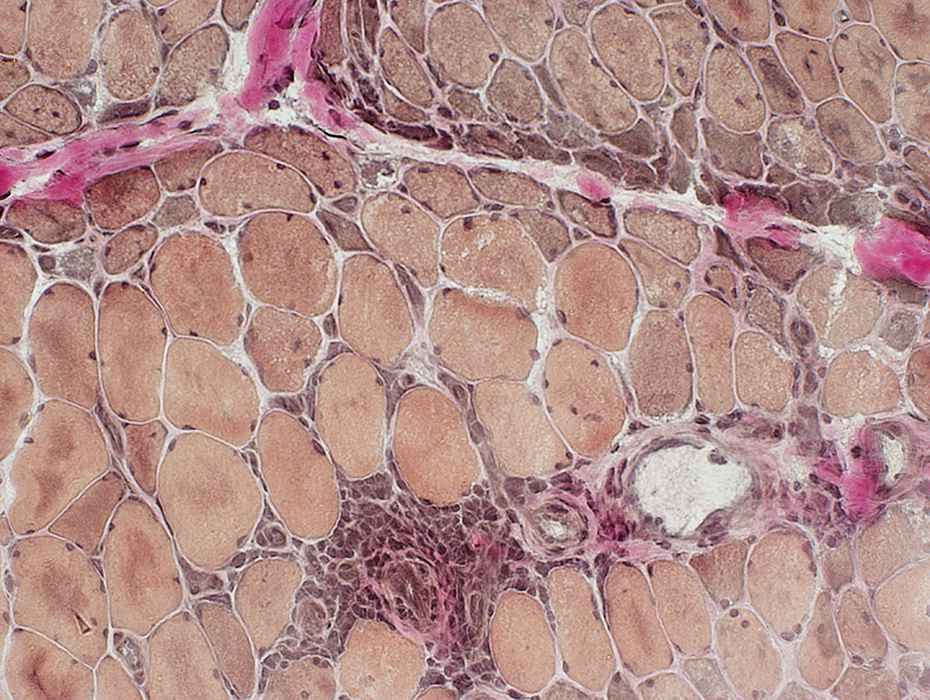 VvG stain |
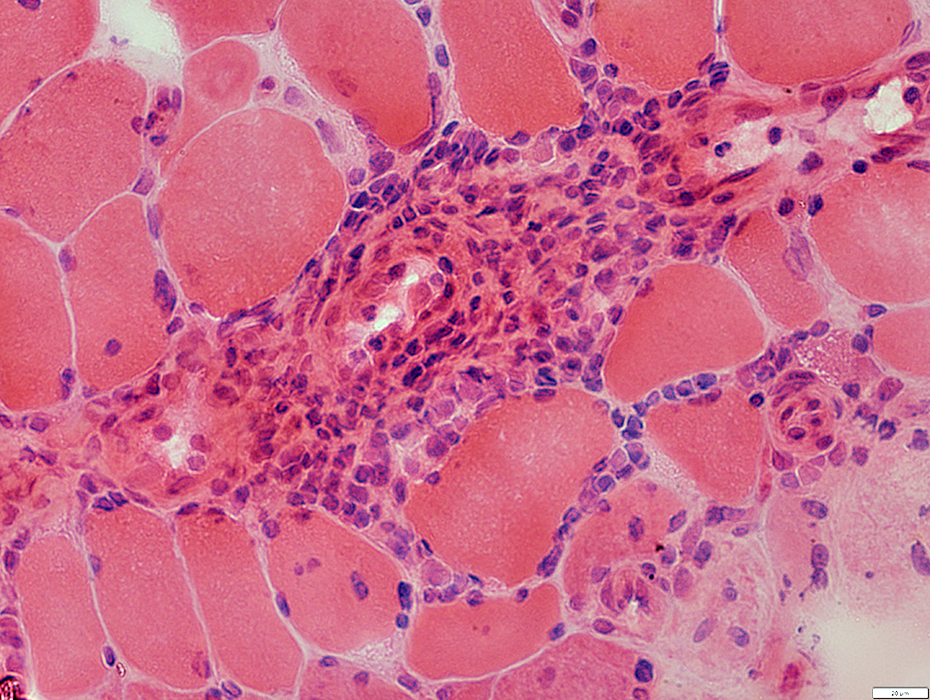 H&E stain |
Cell types: Lymphocytes + Scattered histiocytes
Location: Perimysium
Also Contain: Intermediate-sized vessels
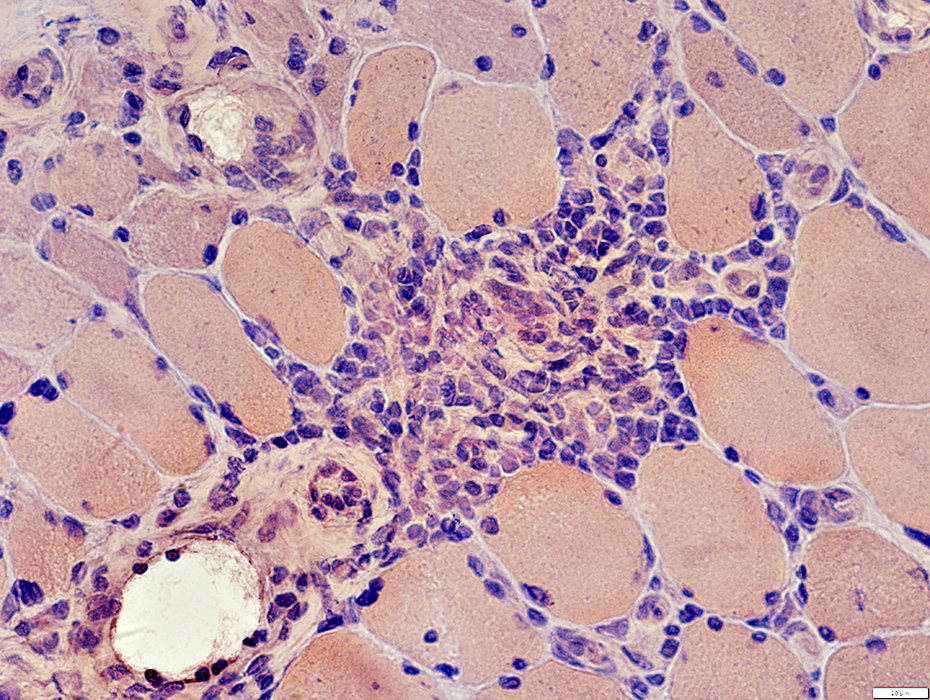 Congo Red stain |
Lymphocyte foci contain: Intermediate sized vessels
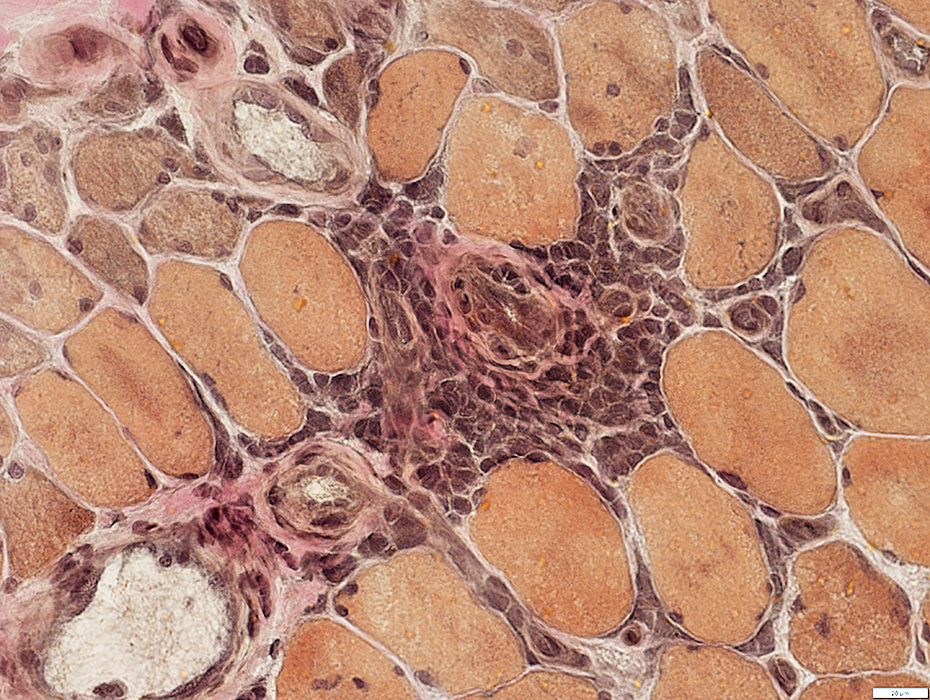 VvG stain |
Cell foci: Contain scattered histiocytes (Acid phosphatase +)
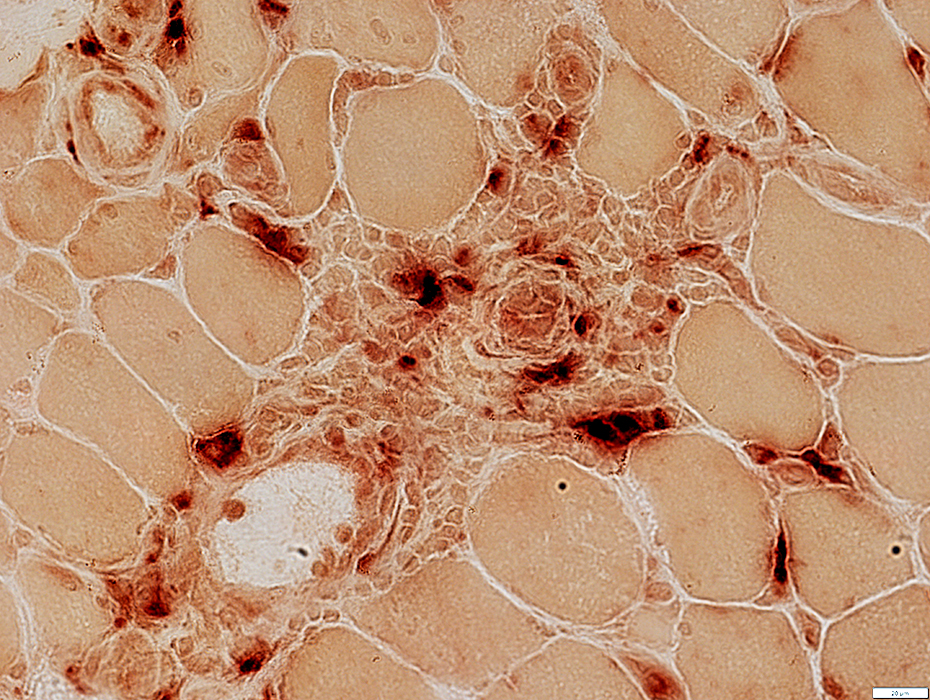 Acid phosphatase stain |
Vessels in cell foci (Arrow): Endothelial cells often stain for esterase
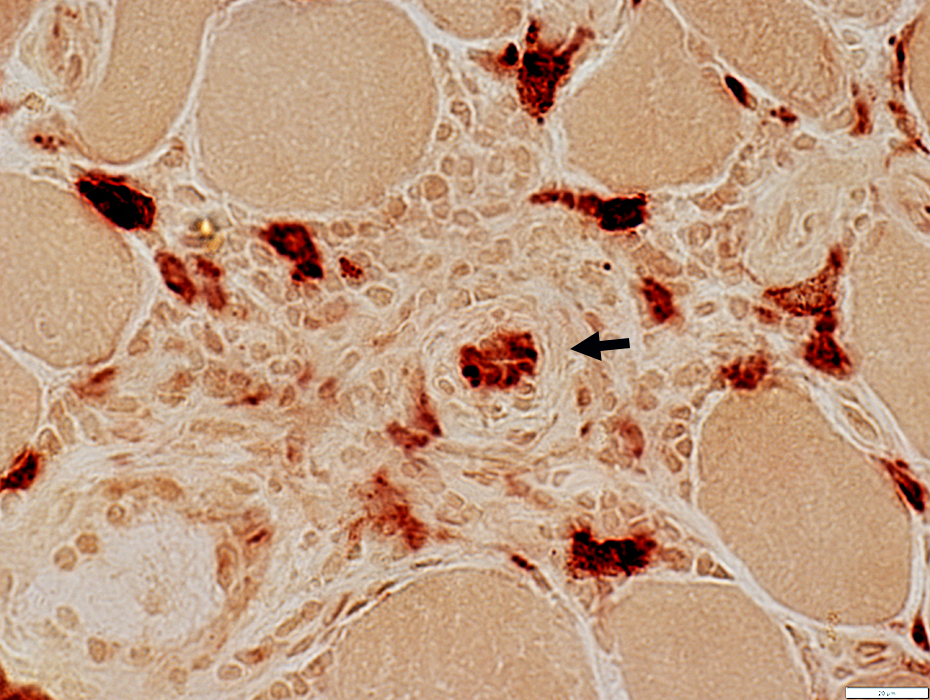 Esterase stain |
|
Mononuclear cell inflammation: Foci Cell types: Lymphocytes + Scattered histiocytes Location Perimysium Distant from muscle fiber atrophy Contain: Intermediate-sized vessels 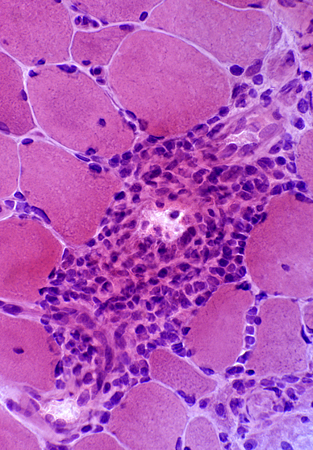
 H&E stain |
 H&E stain |
|
Mononuclear cell inflammation: Stains for CD4 and, in some regions, CD20 (B-cells) Commonly perivascular. | ||
 CD4 stain |
 CD20 stain |
 Congo red stain |
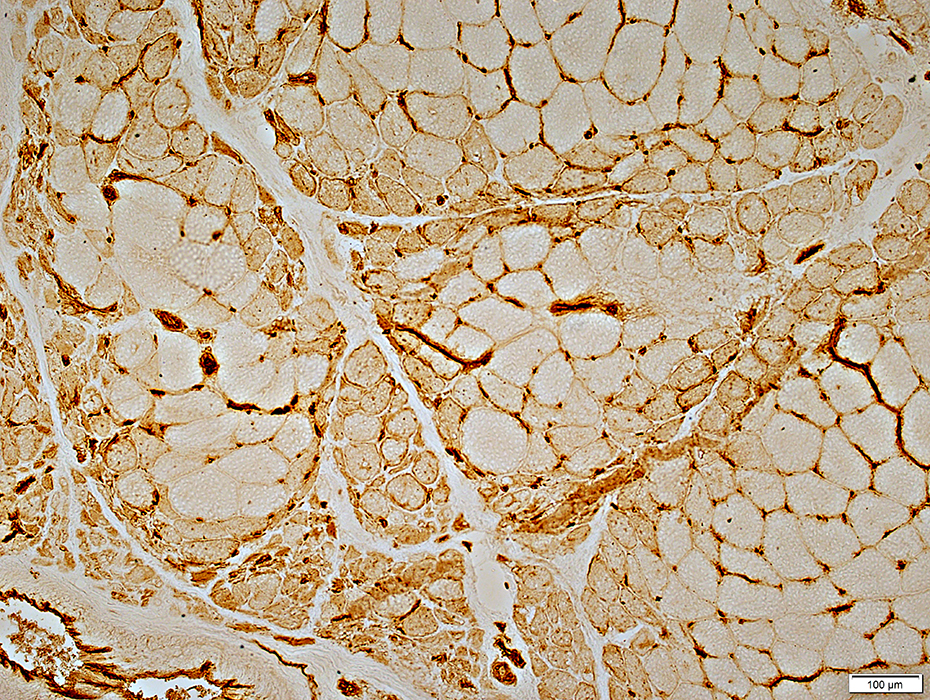
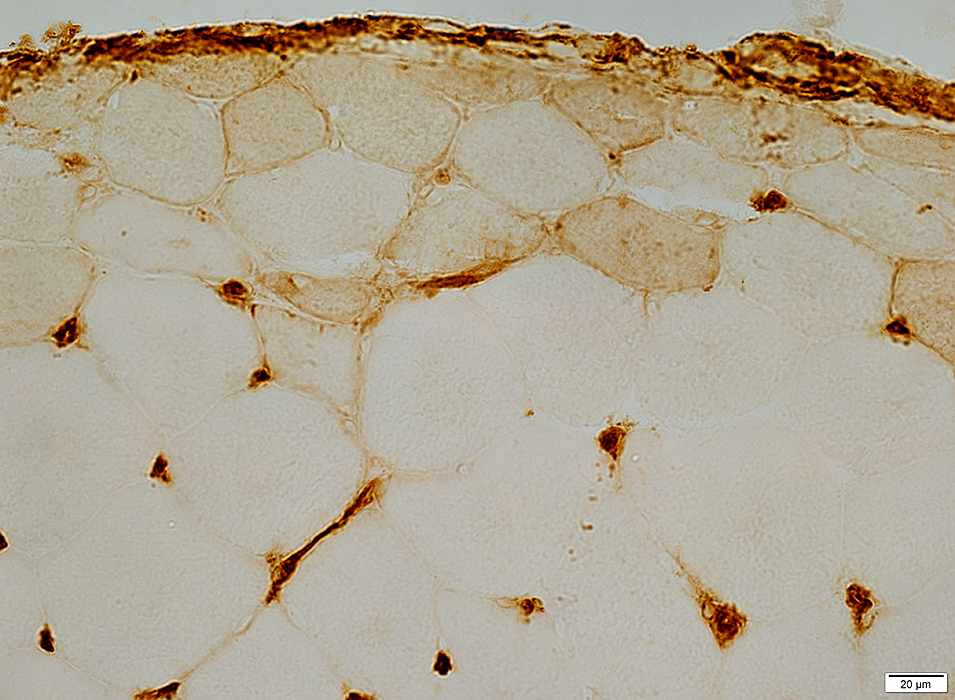
Childhood dermatomyositis (DM-VP): Capillary pathology
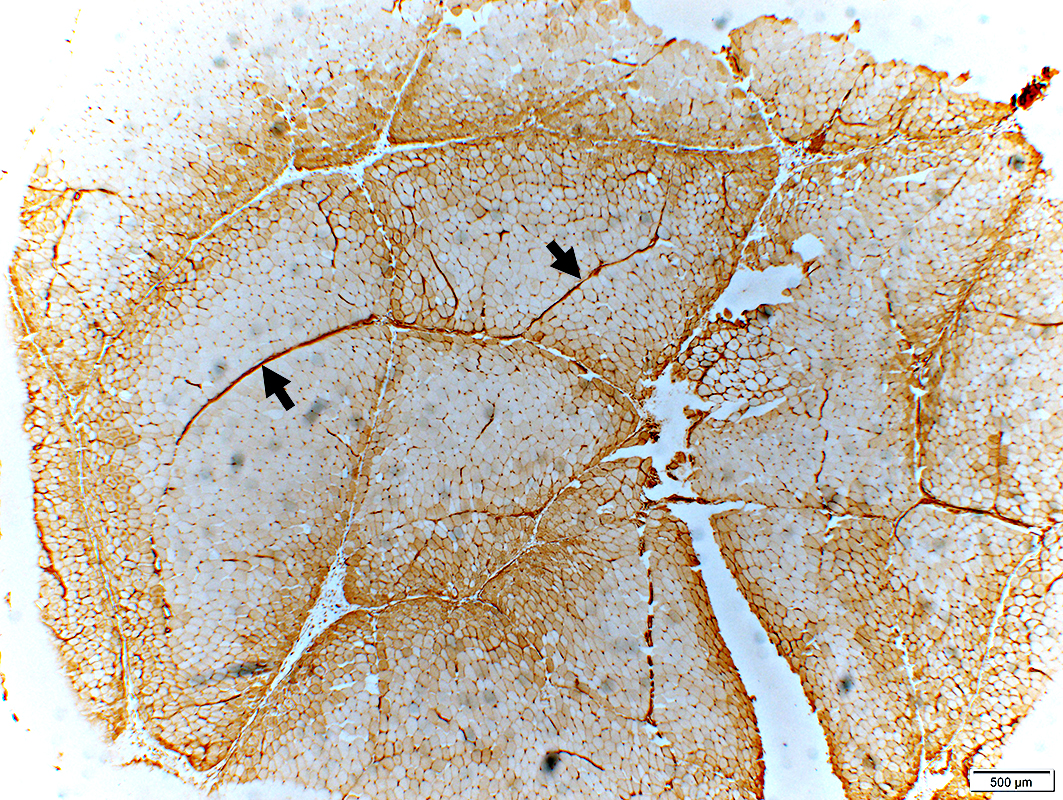
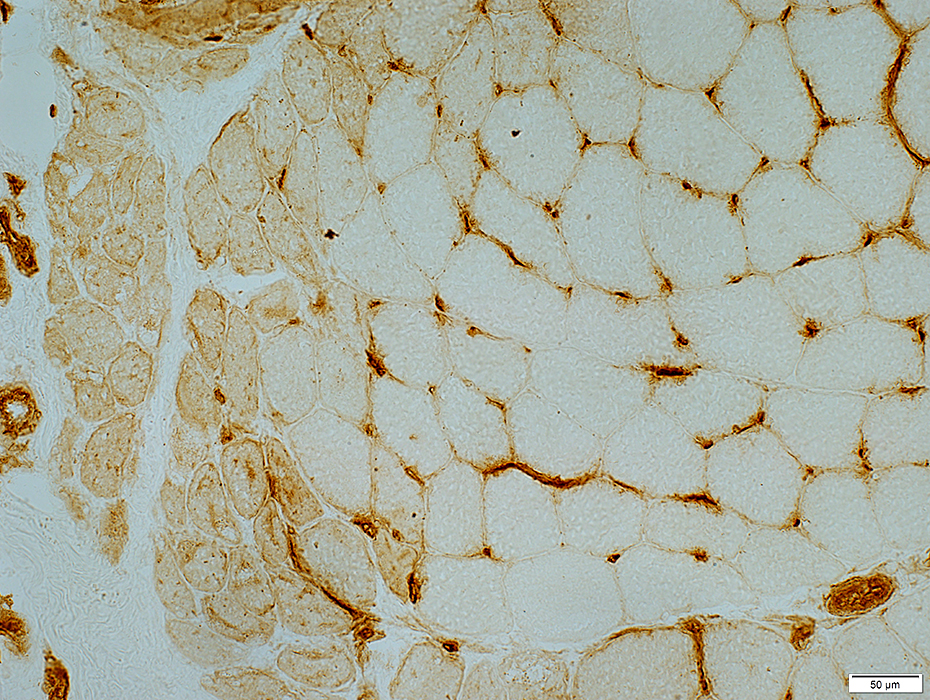
Capillaries: Ulex staining of Endothelium
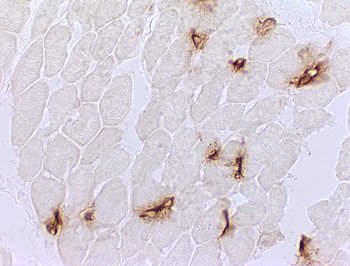
 Stain: Ulex europaeus agglutinin I Dermatomyositis: Capillaries Capillary pathology is patchy and most prominent in perifascicular regions. Capillary staining with Ulex lectin is often absent in regions with small perifascicular muscle fibers (Above left). Capillaries in regions near perifascicular atrophy are often enlarged (Above right). |
 Stain: Ulex europaeus agglutinin I |
 Stain: Ulex europaeus agglutinin I Control: Capillaries are abundant and small CAPILLARY PATHOLOGY: Regional 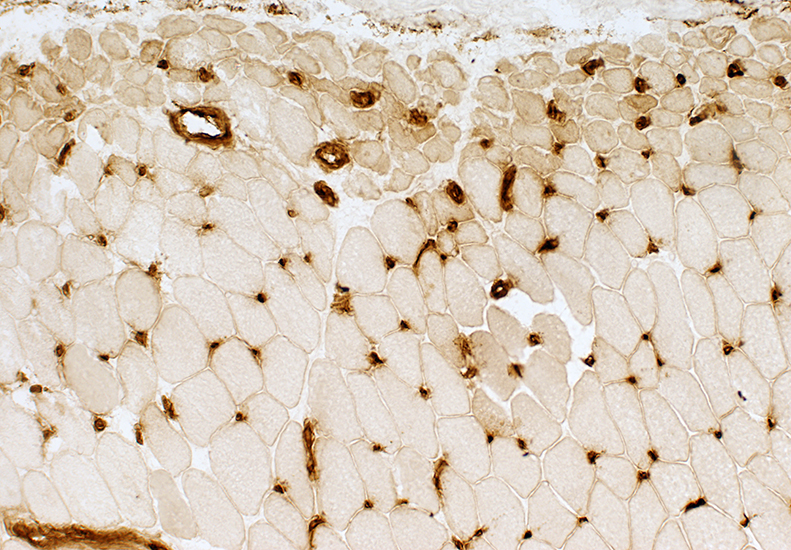 Stain: Ulex europaeus agglutinin I (UEAI) Muscle fiber atrophy (Top) Few stained capillaries Many muscle fibers with no adjacent capillary. Region neighboring muscle fiber atrophy (Purlieu; Middle & Below) Enlarged capillaries Increased staining for alkaline phosphatase; Also see Region distant from muscle fiber atrophy: Capillaries have nearly normal size and number Endomysial capillaries in region neighboring muscle fiber atrophy (Purlieu): Abnormal staining for alkaline phosphatase: Also see 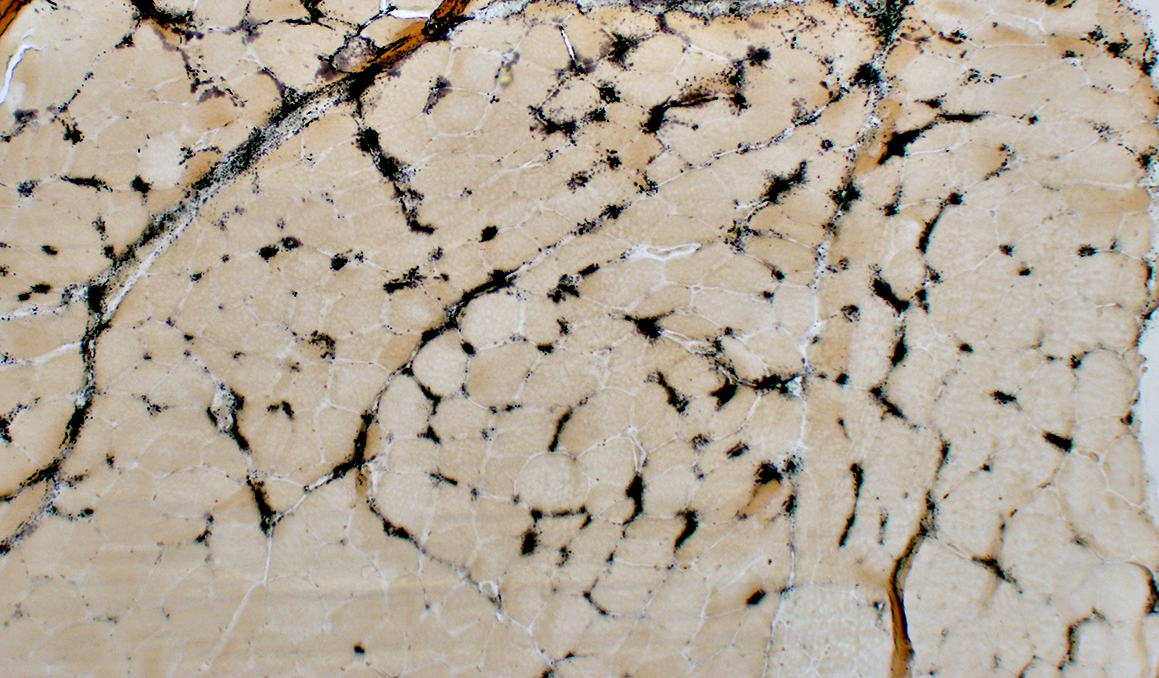 Alkaline phosphatase stain |
Alkaline Phosphatase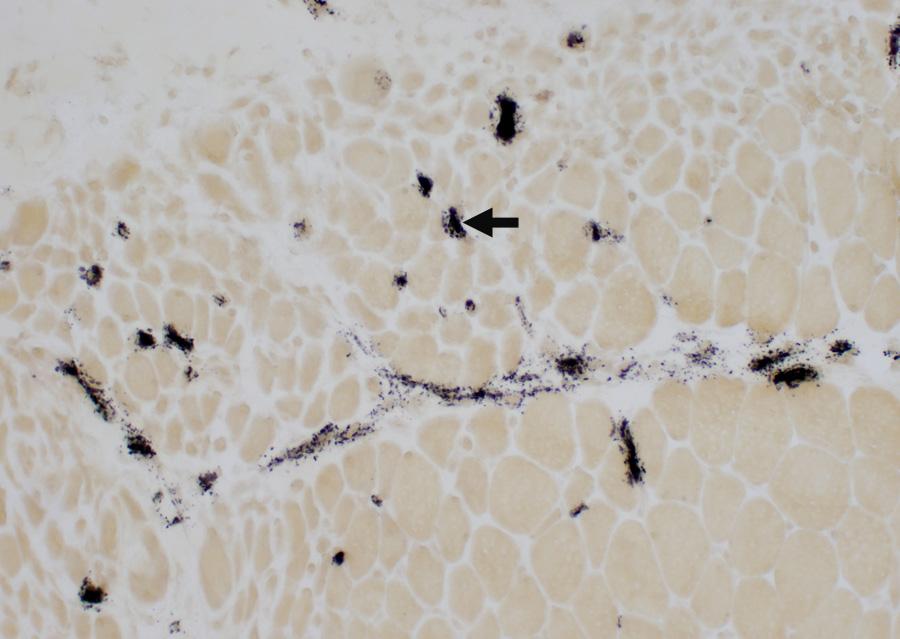 Enlarged capillaries (Arrows): In regions neighboring the smallest muscle fibers: Also see Fewer capillaries stain among larger fibers or amid the smallest fibers at the edge of fascicles. 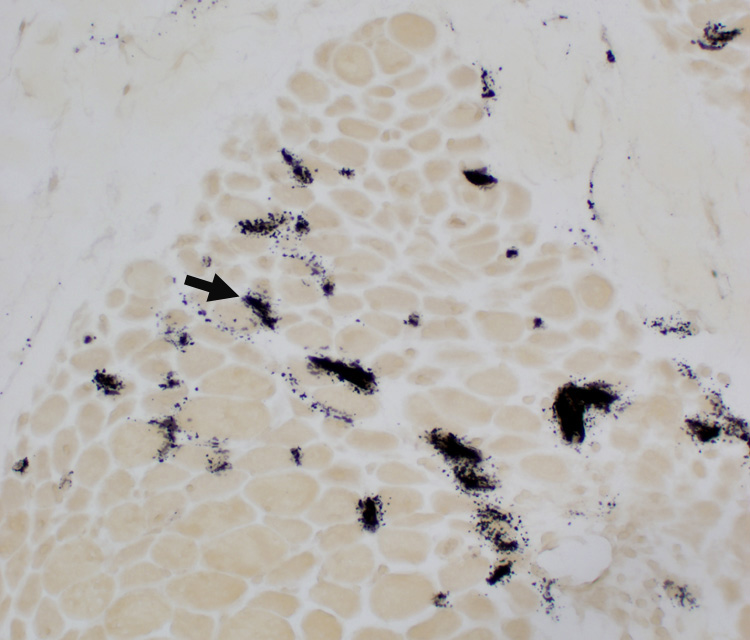 Alkaline phosphatase stain |
|
Endomysial Capillaries Alkaline phosphatase Staining: Especially in perifascicular regions | ||
 Alkaline phosphatase stain |
 Alkaline phosphatase stain |
|
Capillaries: PECAM-1 & Collagen IV stains
|
Normal capillaries Dermatomyositis Enlarged capillaries Capillary remnants |
|
NORMAL ENDOMYSIAL CAPILLARIES Ultrastructure Endothelium + Collagen IV Collagen IV: Stains Capillary walls (Red & Yellow) & Basal lamina around muscle fibers (Red). PECAM1: Stains Capillary endothelium in lumens (Green) and overlaps Collagen IV (Yellow) in walls. 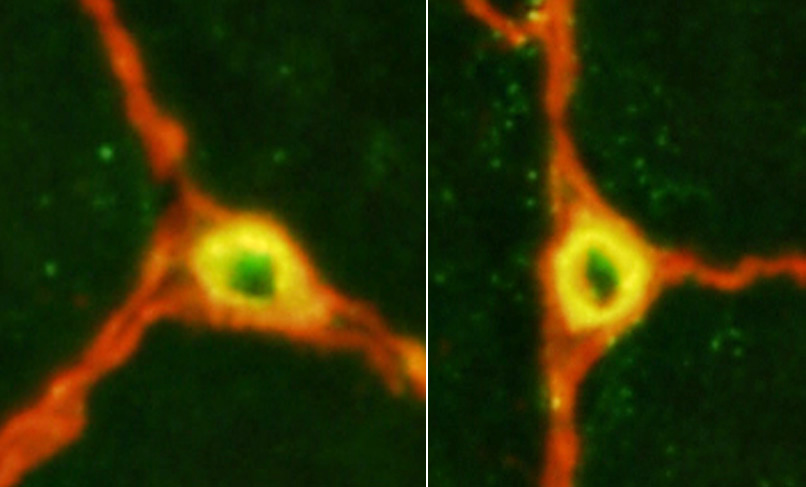
|
|
Capillary amidst Normal muscle fibers: Normal size & morphology. Capillary compositon Endothelial cells (E): Next to lumen Basal lamina: Thick; Surrounds endothelial cellls Pericyte (processes) (P). Red blood cell: In capillary lumen  |
|
Dermatomyositis (DM-VP): SMALL ENDOMYSIAL CAPILLARY REMNANTS in areas of Perifascicular Atrophy Ultrastructure Endothelium + Collagen IV Collagen IV (Red) stains small capillary wall remnants (Arrow) without lumens. PECAM1 stains little, or no, capillary endothelium. 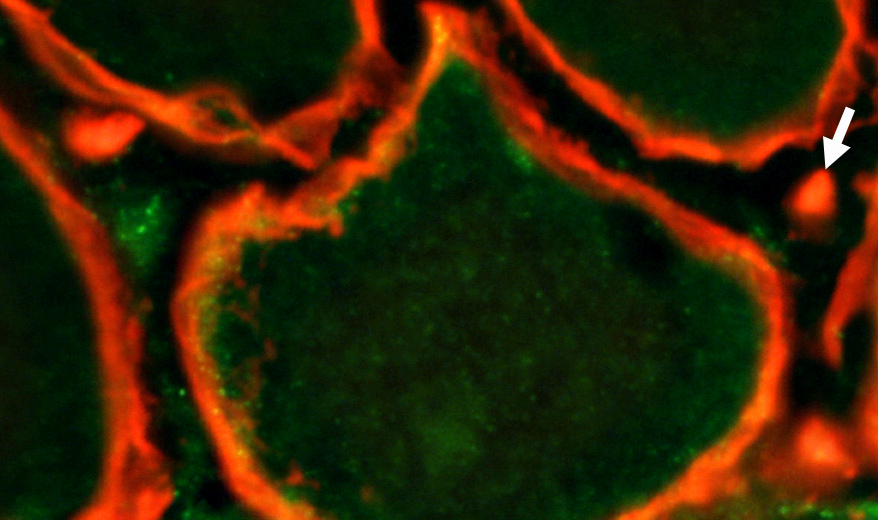 Pericytes & Cells + Collagen IV Collagen IV (Red & Yellow) stains round capillary remnants and basal lamina around muscle fibers. PDGFRβ stains capillary pericytes (Yellow) overlapping Collagen IV & elongated endomysial cells (Green). 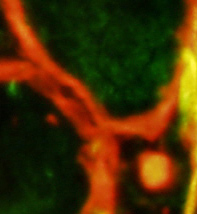
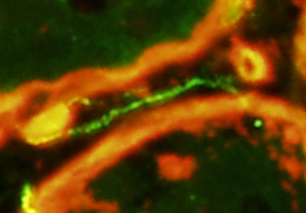
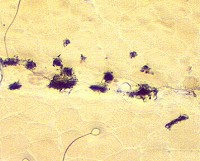
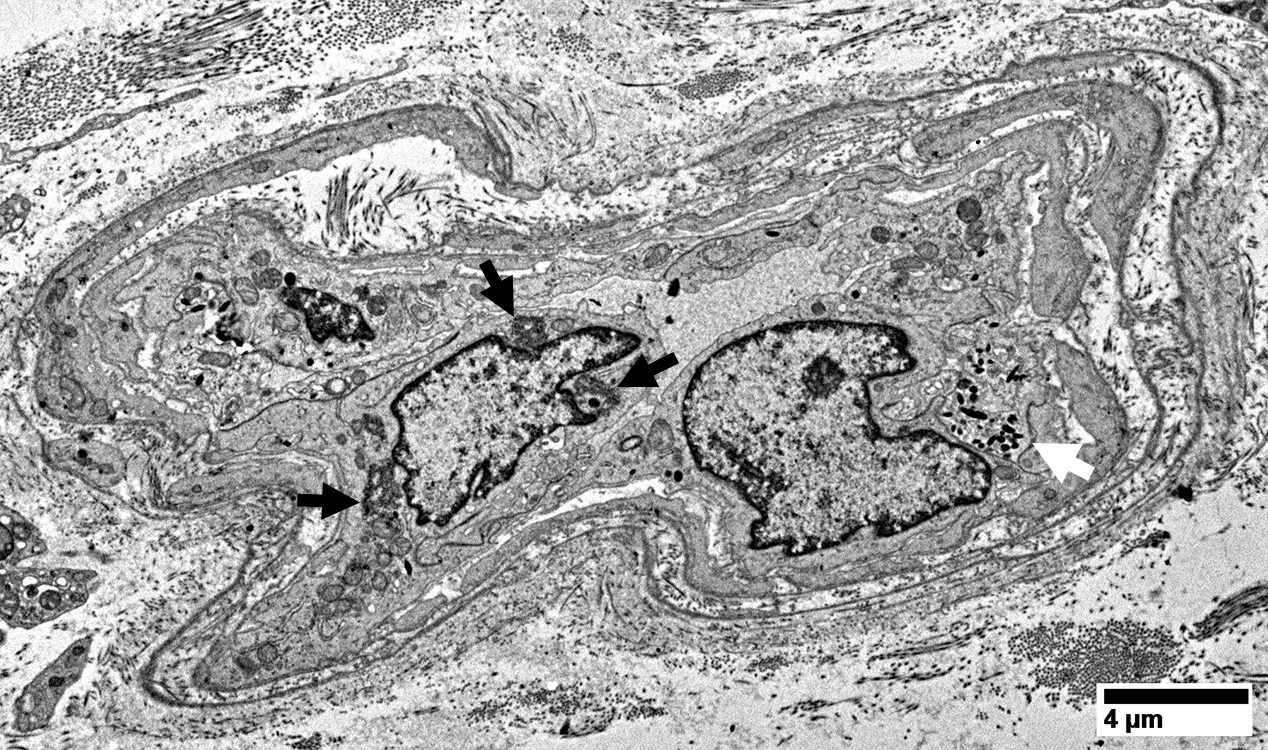
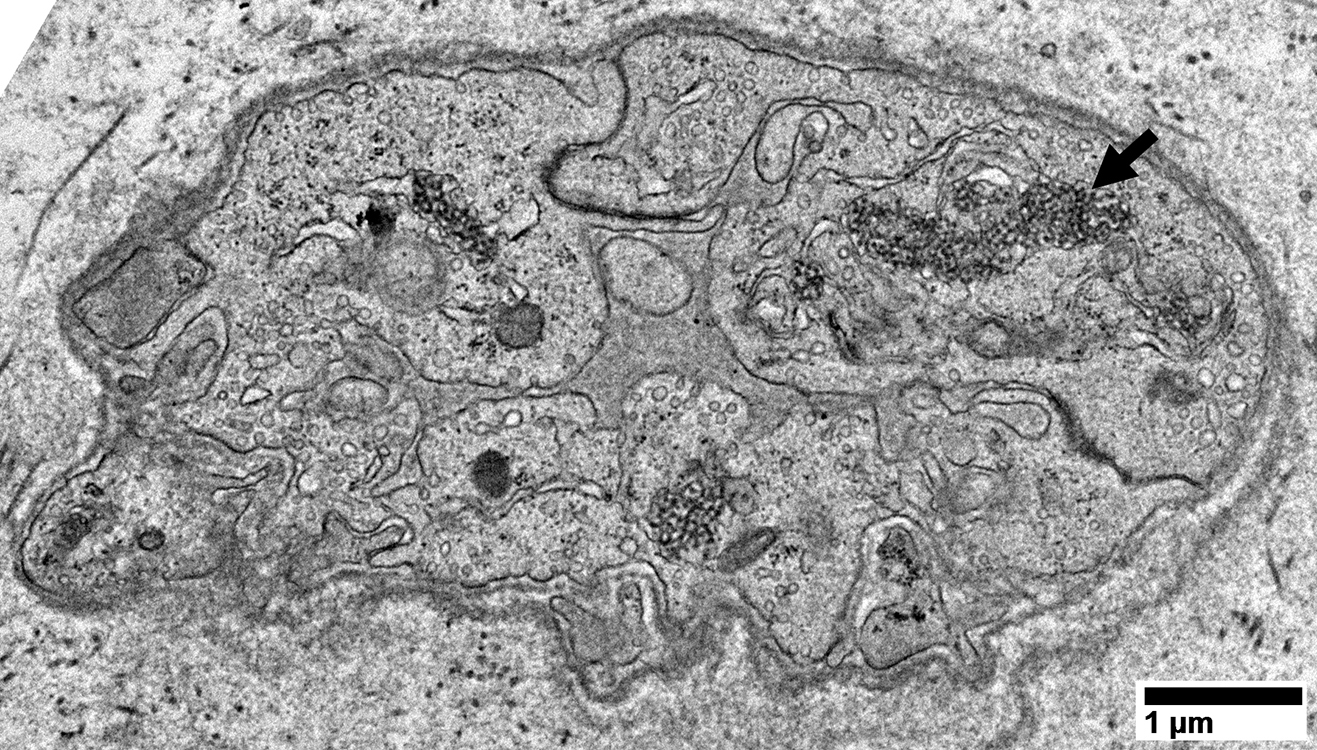
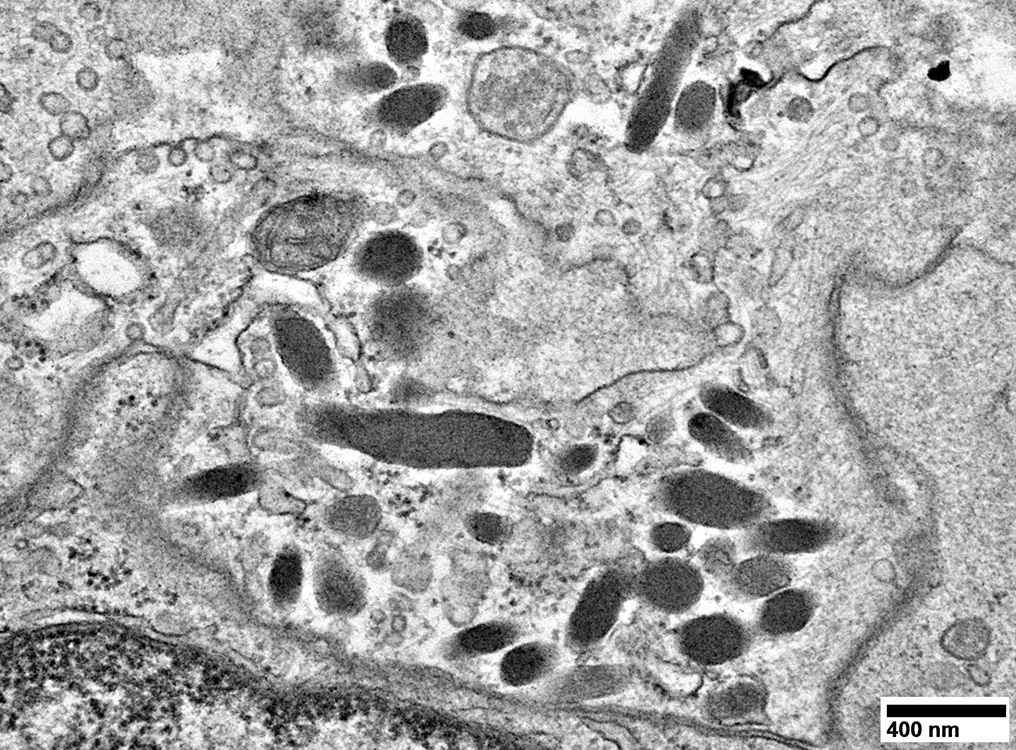
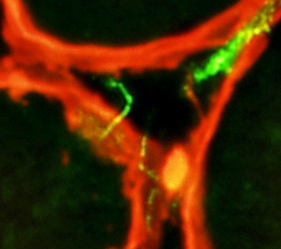 Dermatomyositis (DM-VP): Capillary Ultrastructure
Capillary in area of Perifascicular atrophy: Small endomysial capillary residua (Arrow) Basal lamina Thick Differs from thin basal laminae of nearby muscle fibers (Arrowhead)) Lumen: No endothelium within basal lamina Neighboring Pericyte: Provides evidence of the pathologic vessel's microvascular origin) 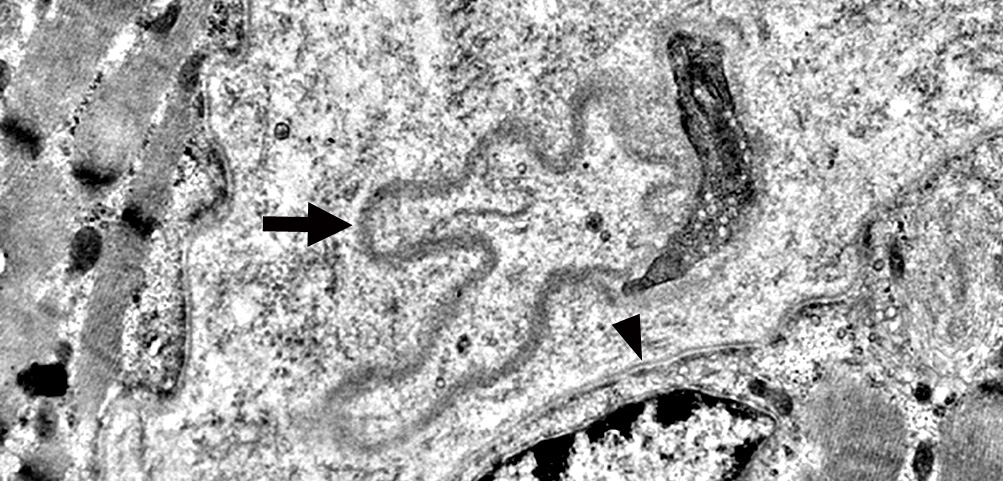 |
|
Dermatomyositis (DM-VP): ENLARGED ENDOMYSIAL CAPILLARIES Ultrastructure Location: Near regions of Perifascicular Atrophy Endothelium + Collagen IV stains Collagen IV: Capillary walls (Red & Yellow) & Basal lamina around muscle fibers (Red). PECAM1: Capillary endothelium in lumens (Green) & Some overlaping Collagen IV (Yellow) in walls. 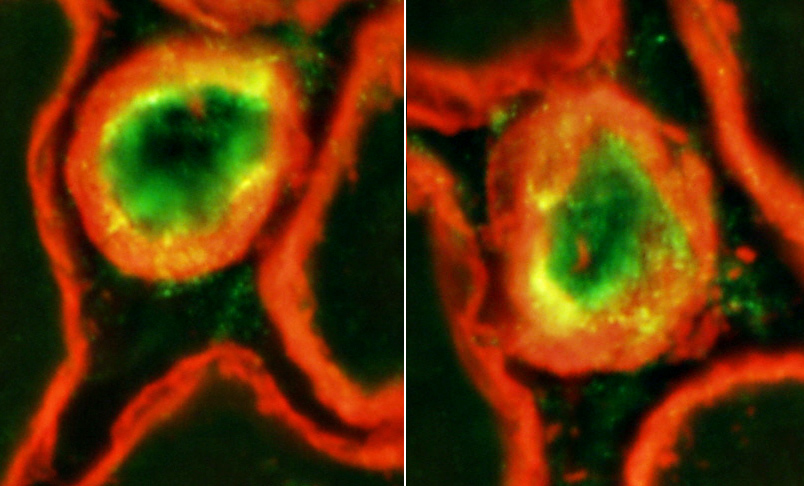
|
|
Enlarged endomysial capillaries (Arrows) Location: Neighbor regions of perifascicular muscle fiber pathology . 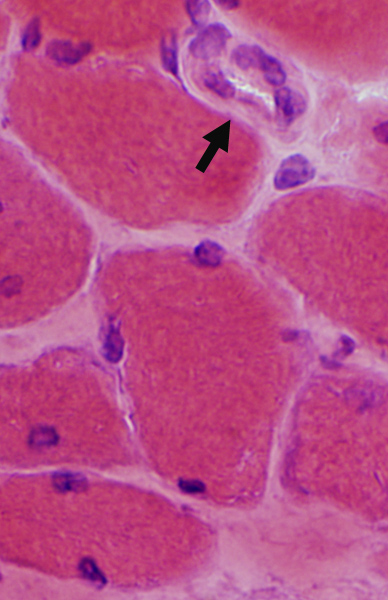
 H&E stain |
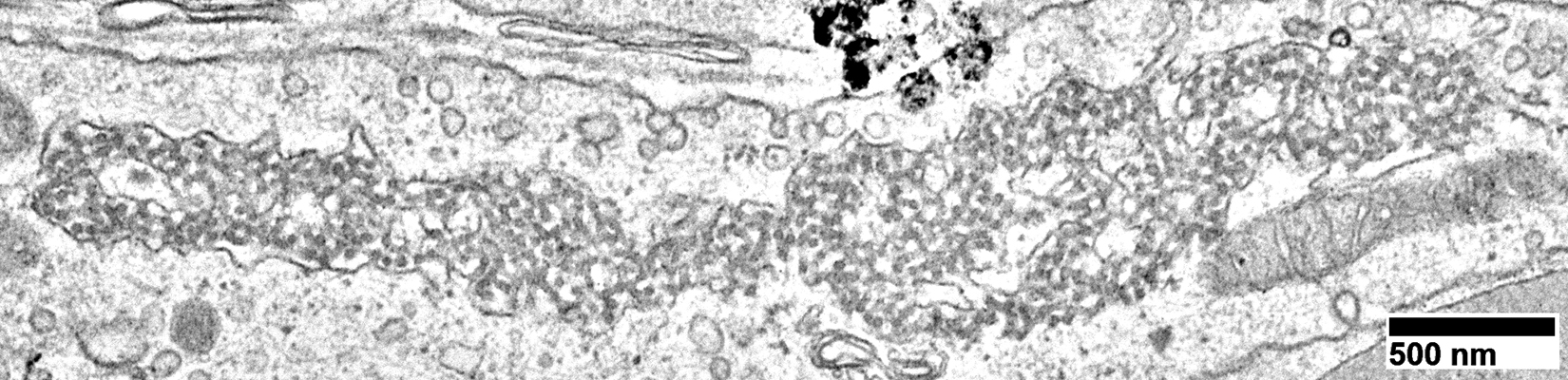
Capillaries in Intermediate zones
Size: Enlarged
Endothelial cells
Size: Enlarged & Abundant cytoplasm
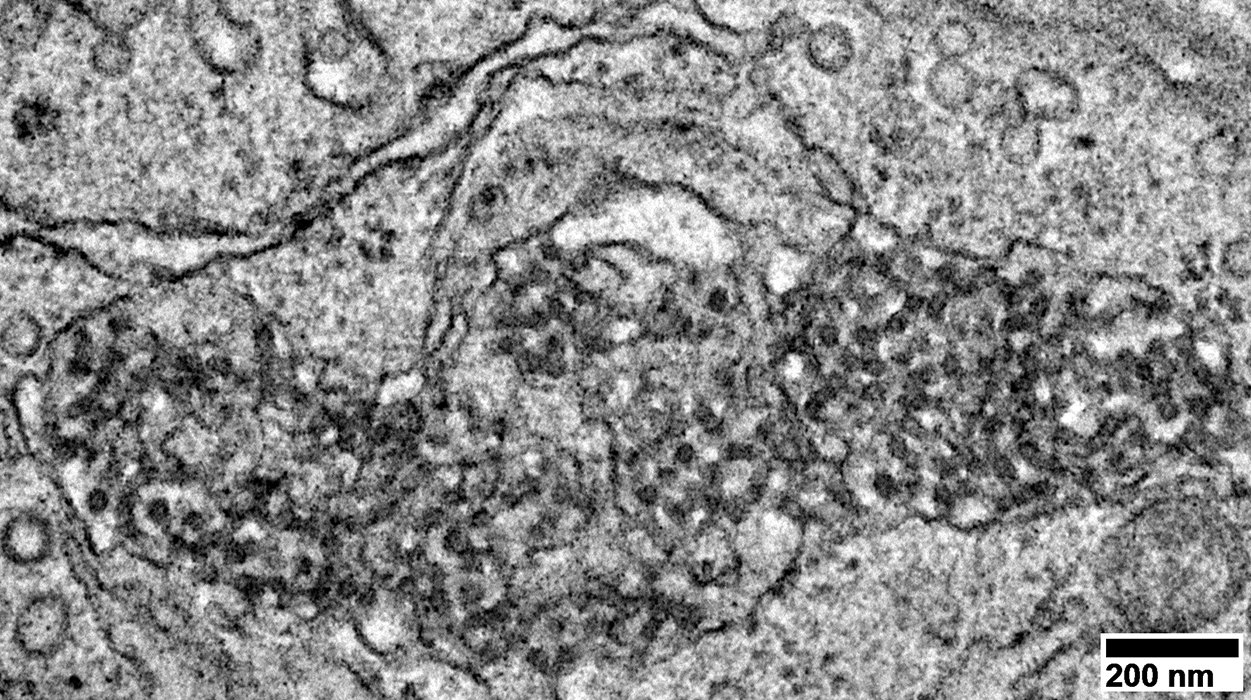
Tubular reticular profiles (Dark arrows): Present in cytoplasm
Abnormal mitochondria (White arrow): Present in some cells
Capillary components
|
|
Location: Cytoplasm of capillary endothelial cells
Continuous with: Endoplasmic reticulum
|
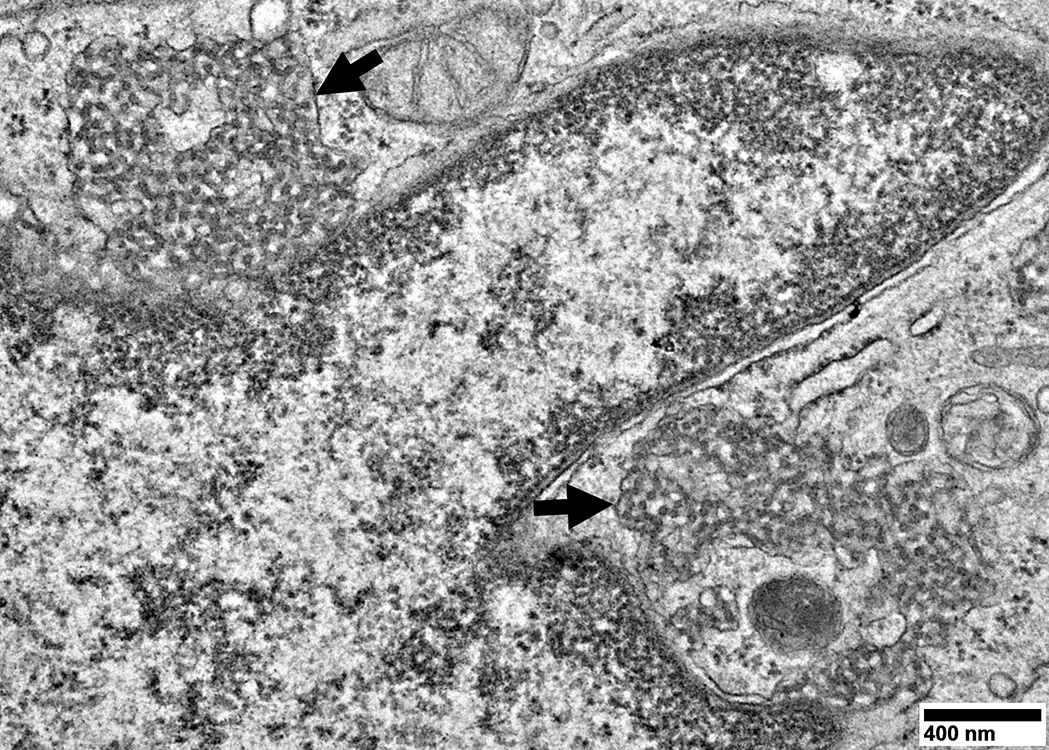
Endothelial cells have
Abundant cytoplasm
Tubular reticular structures (Arrow)
|
Tubular Reticular Structures
|
Endothelial cell cytoplasm: Contains Mitochondria & Weibel Palade bodies
|
Structure: Elongated, cigar-like shape (0.2 μm in width; Up to 4 μm in length)
Location: Endothelial cells
Function: Secretory organelles; May be exocytosed
Contents: Proteins that contribute to inflammation, angiogenesis & tissue repair
von Willebrand factor (VWF)
Other
tPA, P-selectin, Interleukin-8 (IL-8), Eotaxin-3, Angiopoietin-2
Osteoprotegerin, Endothelin-1, Endothelin-converting enzyme, Calcitonin gene-related peptide
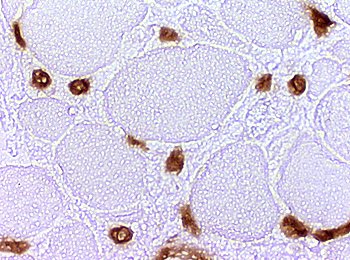
Childhood dermatomyositis (DM-VP): Complement (C5b-9) deposition on Endomysial capillaries
 Stain: C5b-9 components of complement (Membrane attack complex) Dermatomyositis: C5b-9 deposition in endomysial capillaries Changes are patchy and most prominent in perifascicular regions amid small muscle fibers. C5b-9 is deposited on damaged endomysial capillaries that have often lost their endothelium. |
 Stain: C5b-9 components of complement (Membrane attack complex) Normal control No C5b-9 deposition in endomysial capillaries in control muscle |
 C5b-9 stain |
C5b9 complement compared to PECAM1 staining of Punctate Capillary Remnants
- LEFT: C5b9 complement staining is present on
- Most punctate Collagen IV endomysial capillary remnants (Yellow)
- Avascular perimysium without Collagen IV (Green) (Large arrowhead)
- RIGHT: Capillary remnants (Red) have no PECAM1 staining (Yellow-Green) (Arrows and many other similar structures)
Endomysial capillaries: C5b-9 complement deposits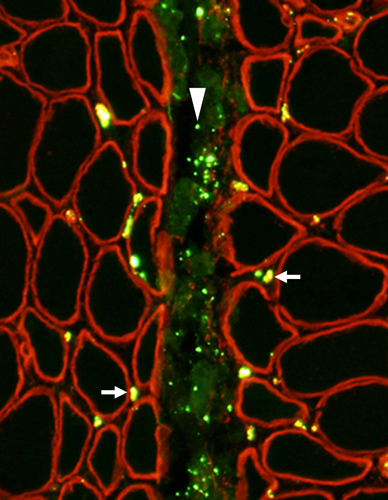 C5b-9 complement (Green) with Collagen IV (Red) |
Endomysial capillaries: No endothelium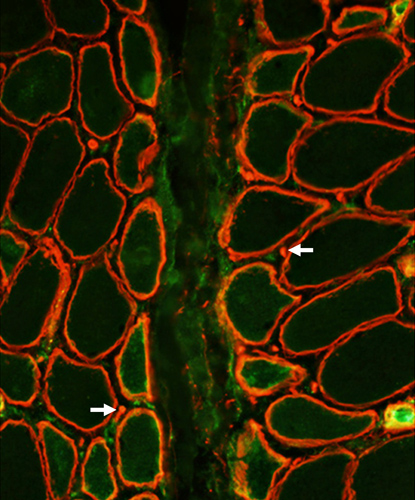 PECAM1 (Green) with Collagen IV (Red) |
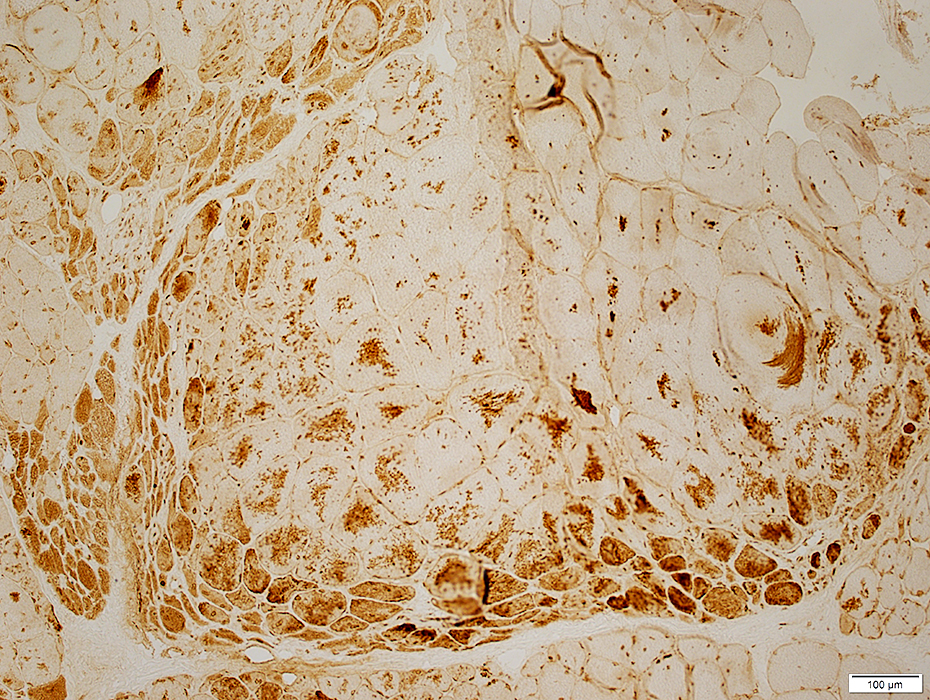
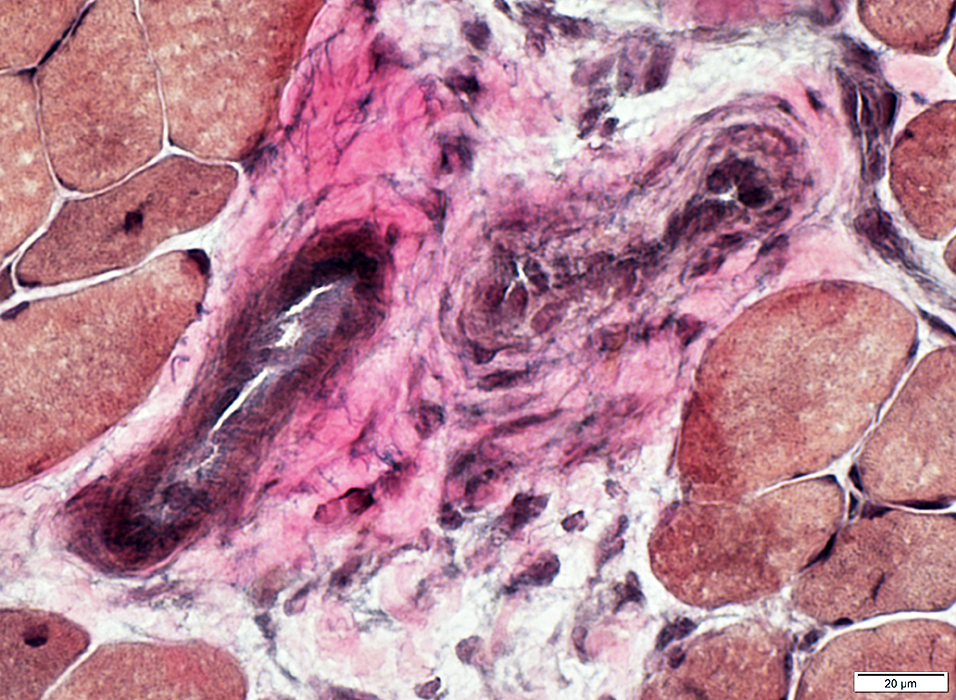
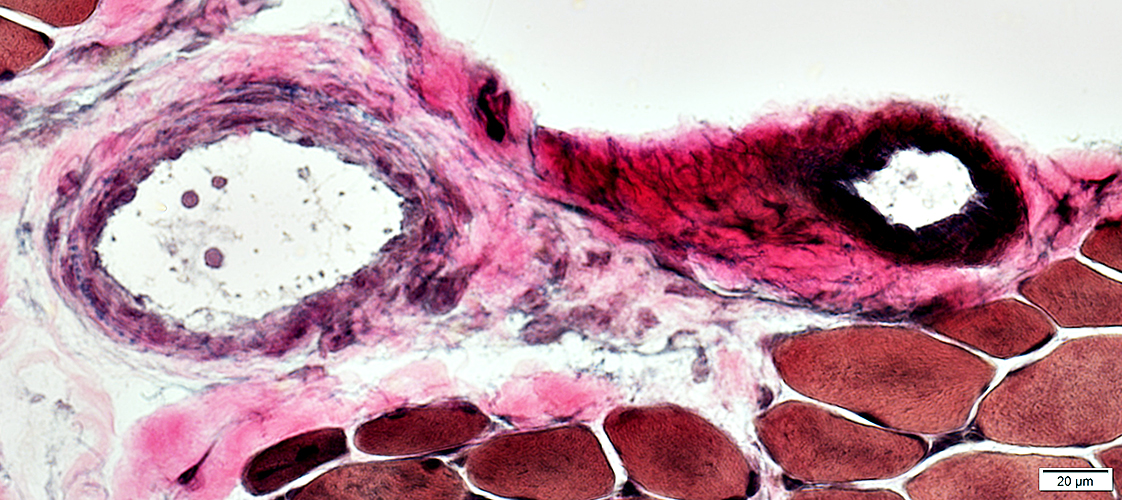
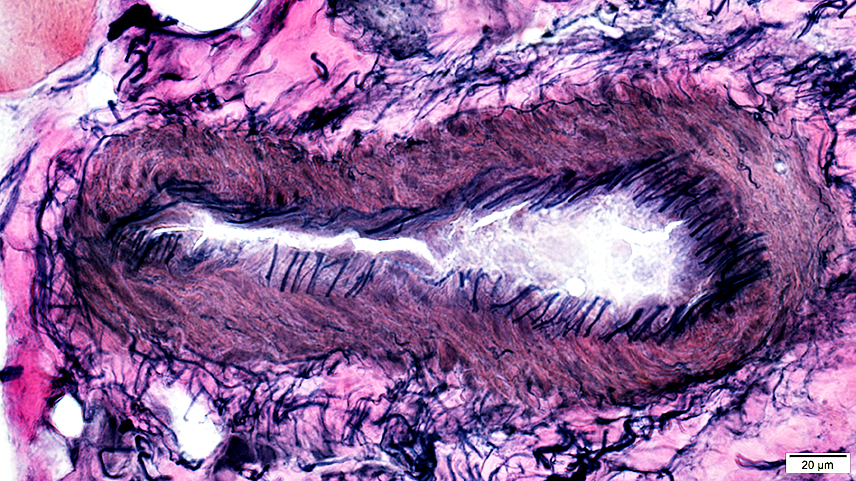
Childhood dermatomyositis (DM-VP): Perimysial Vascular Pathology
|
Vessel walls: Abnormal structure Damaged vessels: Fragments without lumens |
Perimysial Arteries (a) & Veins (v)
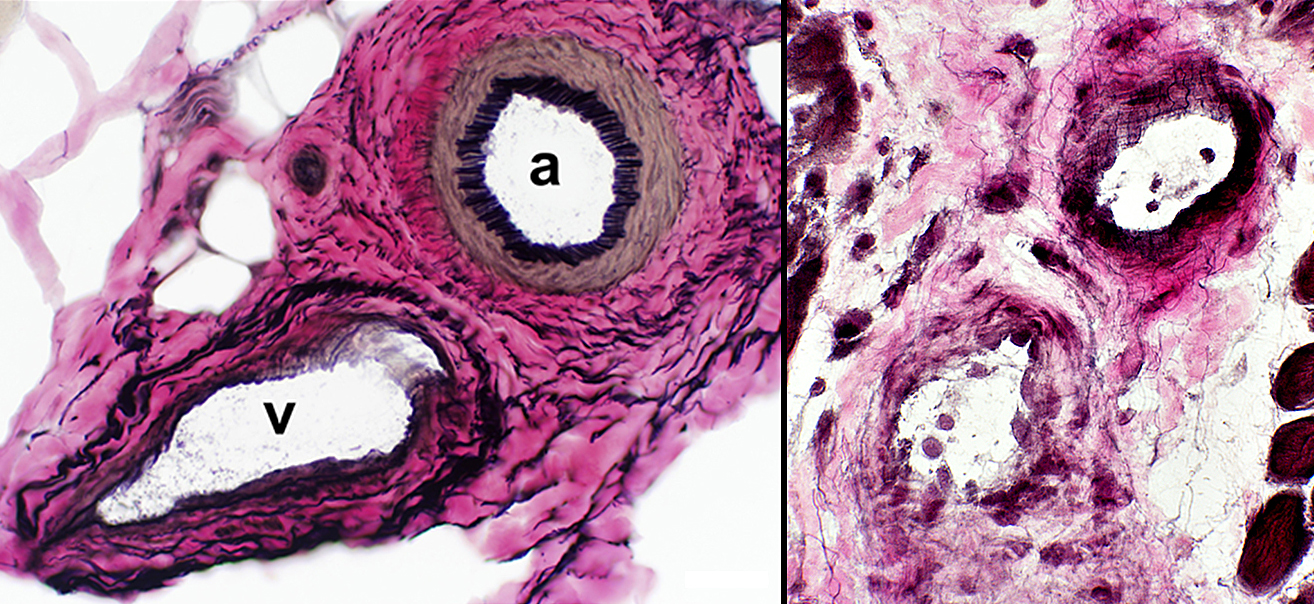 VvG stain |
DM-VP (Above Right & Below)
Loss or thinning of fibrils in walls of arteries & veins
Endothelial cells: Enlarged, May contain tubulo-reticular profiles
 VvG stain |
Fibrils in wall reduced
 VvG stain |
Endothelial cells large
Wall: No fibrils
Perimysial vascular fragments: No lumen
 VvG stain |
|
Dermatomyositis (DM-VP): Vascular Perimysium Contains abnormal vascular fragments (Yellow) Has increased PECAM1 staining Located away from perifascicular muscle fiber atrophy PECAM1 (Green) + Collagen IV (Red): Overlap = Yellow 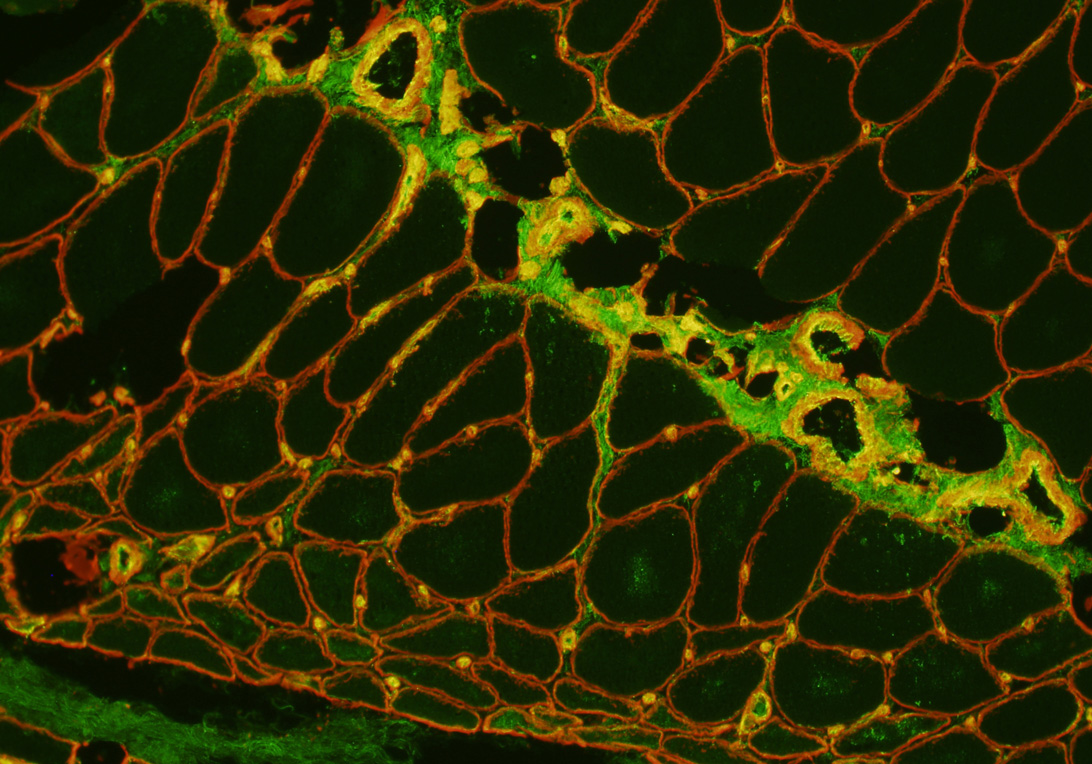
|
|
Normal: Vascular Perimysium Contains normal intermediate-sized vessels with lumens Has minimal PECAM1 staining PECAM1 (Green) + Collagen IV (Red): Overlap = Yellow 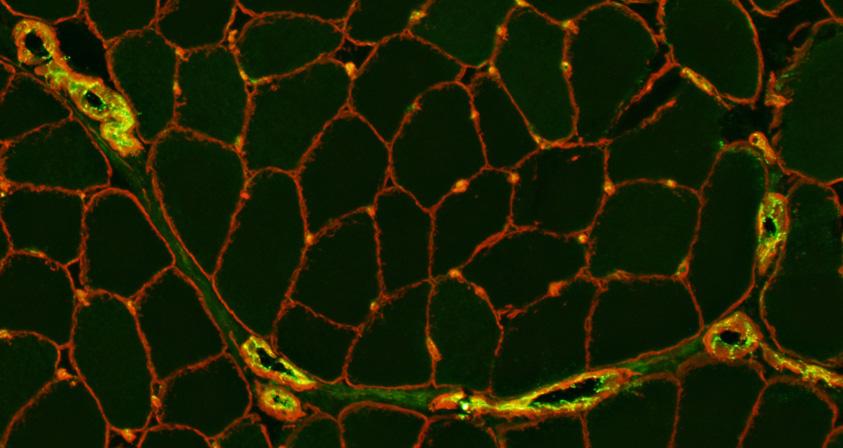
|
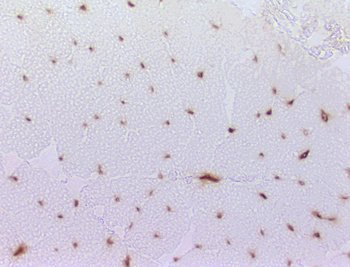
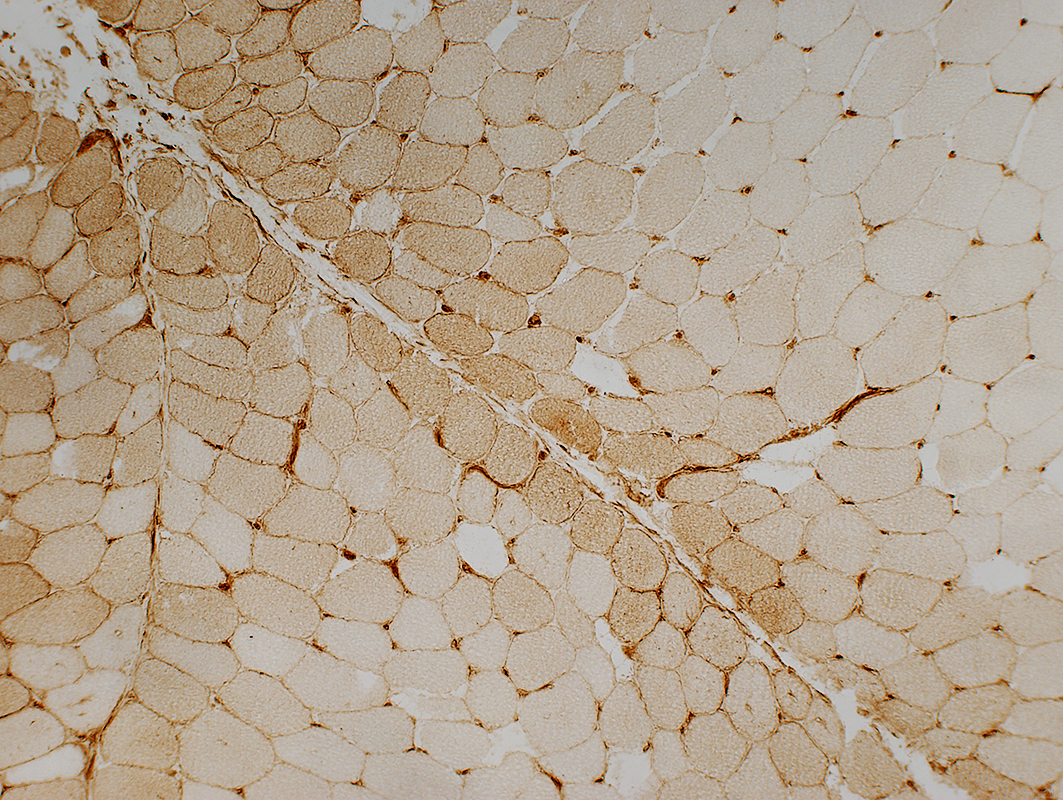
DM-VP (Childhood dermatomyositis): MHC Class I upregulation
|
Distribution Pathology degree Severe Mild |
DM-VP, Moderately severe: MHC-I up-regulation by muscle fibers, more in small fibers at edge of fascicle
 MHC Class I |
 MHC Class I Normal: MHC I not present in muscle fibers. Staining is only on capillaries |
Perifascicular muscle fibers near avascular perimysium express MHC-I
Central muscle fibers near vessel (Arrow; Below) express less, or no, MHC-I
 MHC Class I |
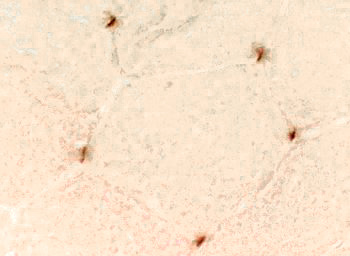
DM-VP, Mild: Patterns of MHC-I staining
MHC-I up-regulation more in muscle fibers at edge of fascicle, or diffusely
Affected muscle fibers may be normal size, or small.
|
MHC Class I upregulation Mild More in muscle fibers in perifascicular region May occur in regions without myofiber atrophy 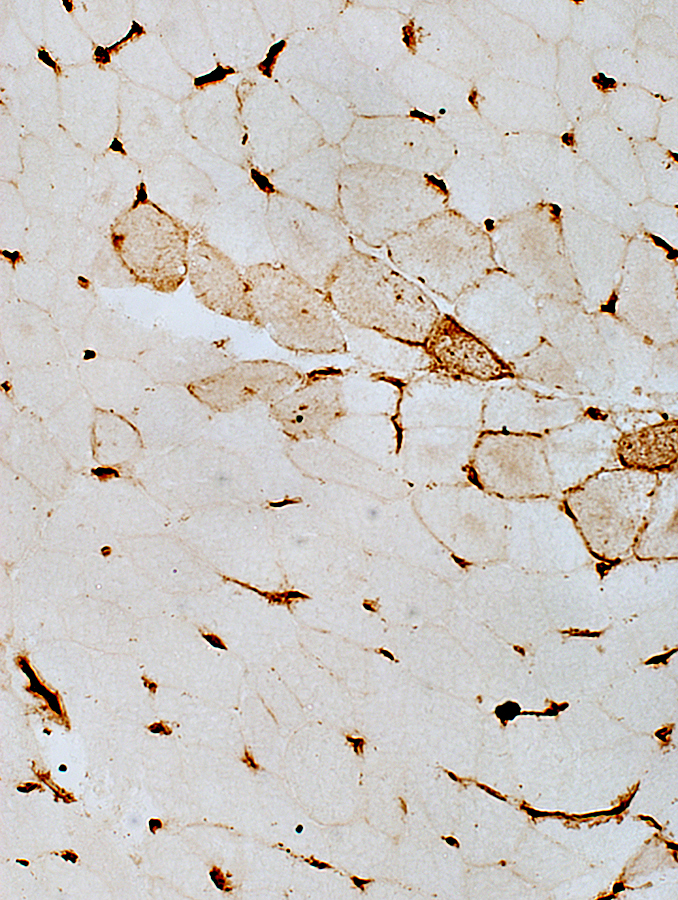
|
DM-VP: MHC I up on muscle fibers especially near perimysium A similar pattern may occur in IMPP syndromes  Stain: MHC Class I |
 MHC Class I stain |
|
MHC Class I upregulation Dffuse Slightly more prominent in perifascicular region May occur in regions without severe myofiber atrophy 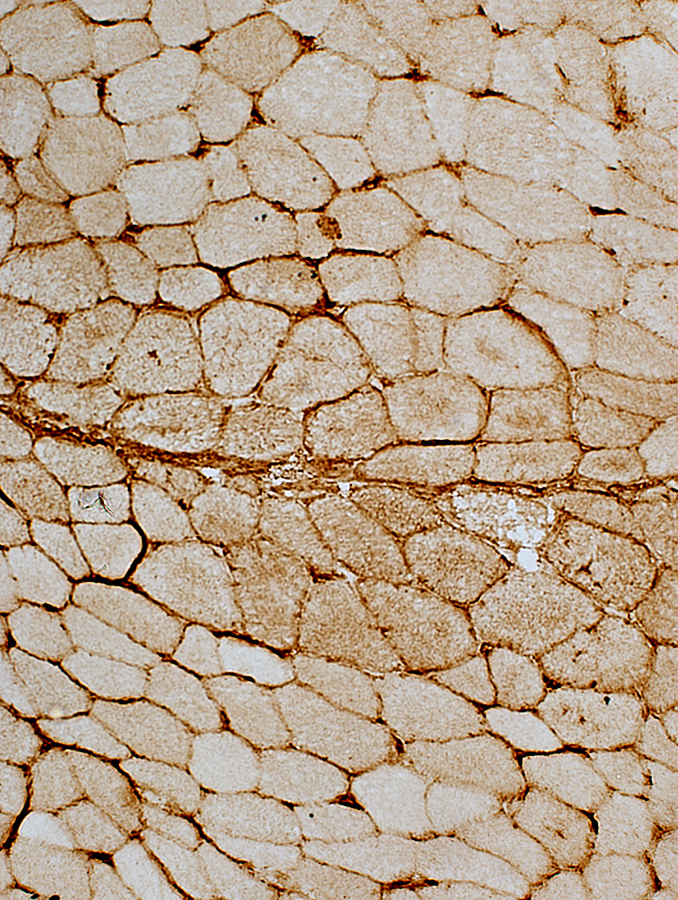
|
DM-VP: MHC I up on muscle fibers, severe Diffusely on the surface and within muscle fibers 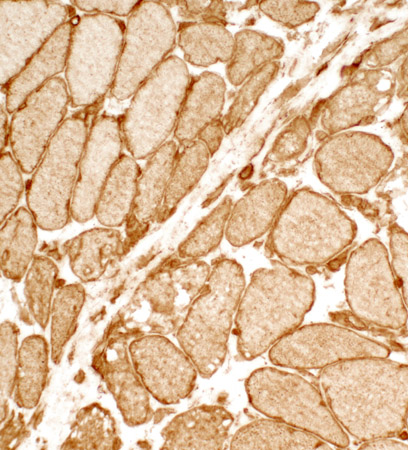 Stain: MHC Class I |
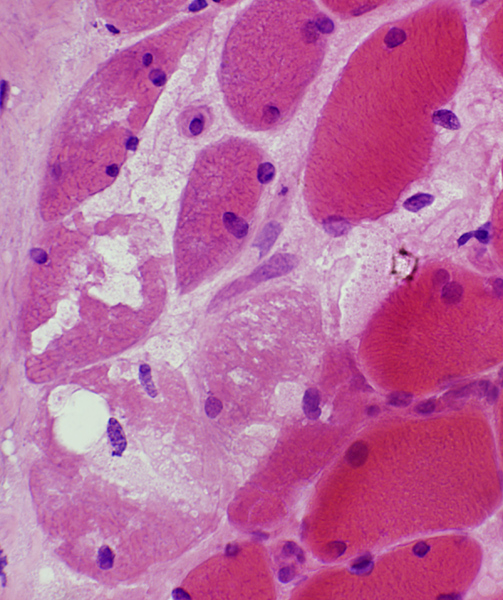
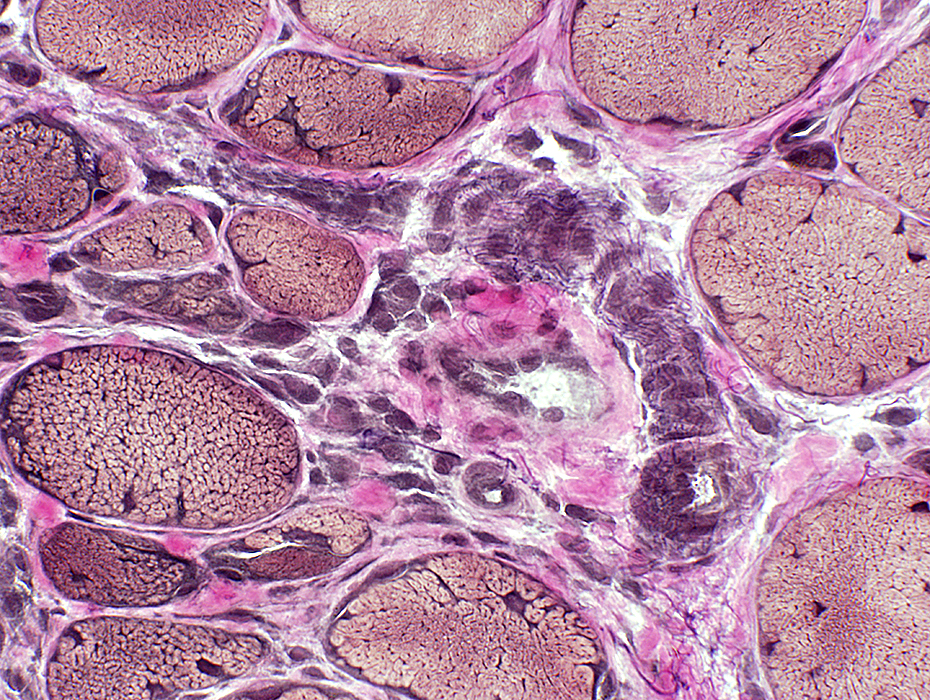
Dermatomyositis with Vascular Pathology (DM-VP): Severe
 H&E stain |
Periphery of Fascicle: Atrophic muscle fibers near avascular perimysium
 VvG stain |
Small Muscle Fibers
 Gomori trichrome stain |
Muscle fibers: Intermediate-sized
Endomysial capillaries: Large
 Gomori trichrome stain |
Near perimysium
Nuclei: Often internal
Surface: Irregular
Cytoplasm: Dark NADH stain
 NADH stain |
 VvG stain |
 VvG stain |
Abnormal structure: Loss of fibrils in arteries & veins
Also see: DM-VP Vessels
 VvG stain |
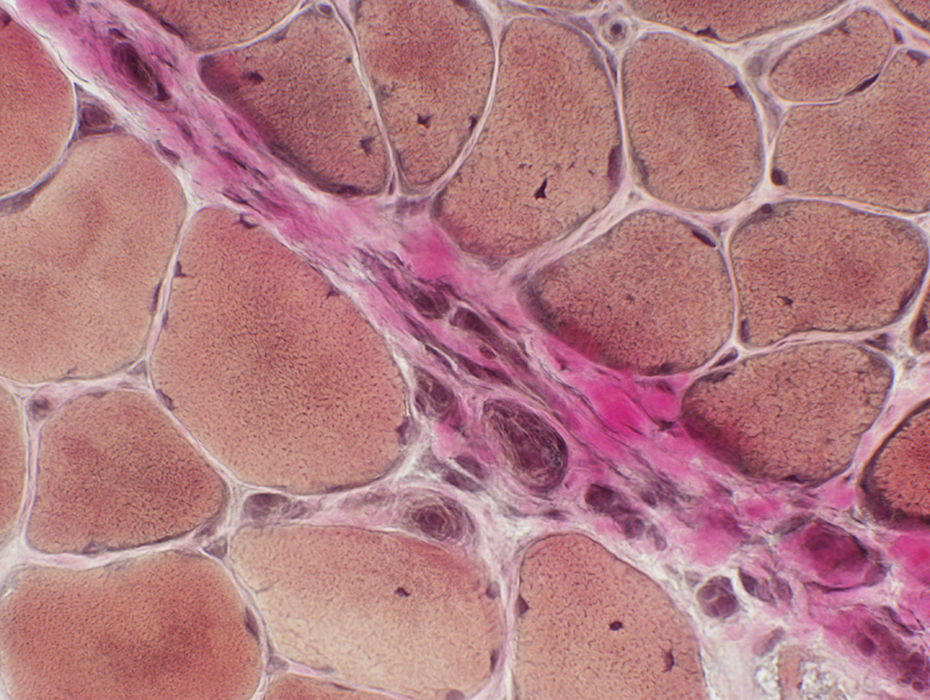
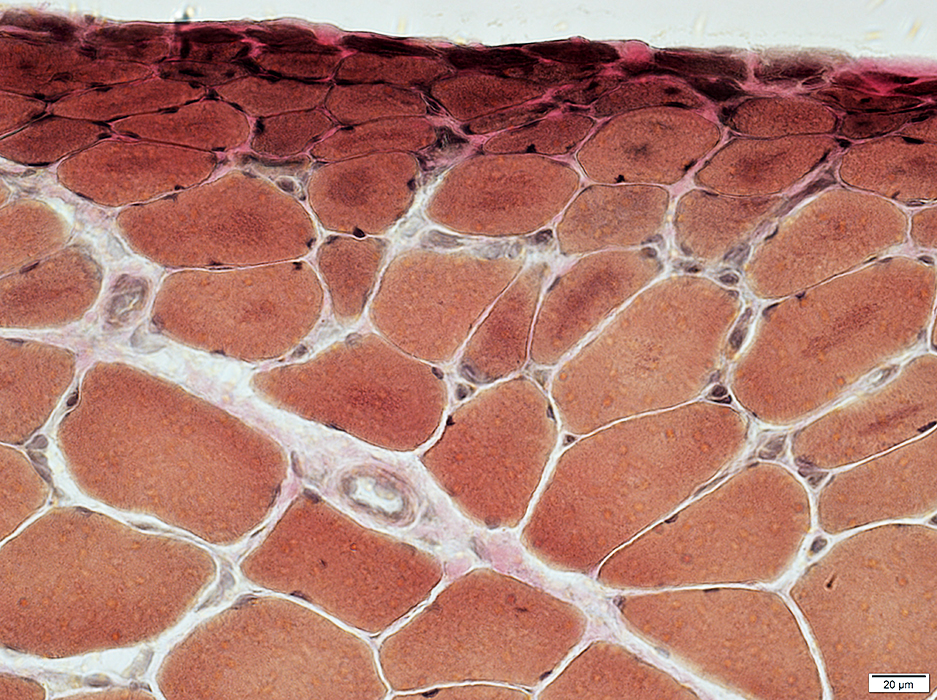
DM-VP (Childhood): Muscle fiber Atrophy at Muscle Surface (Epimysium)
Severe atrophy of muscle fibers at edge of muscle
 H&E stain |
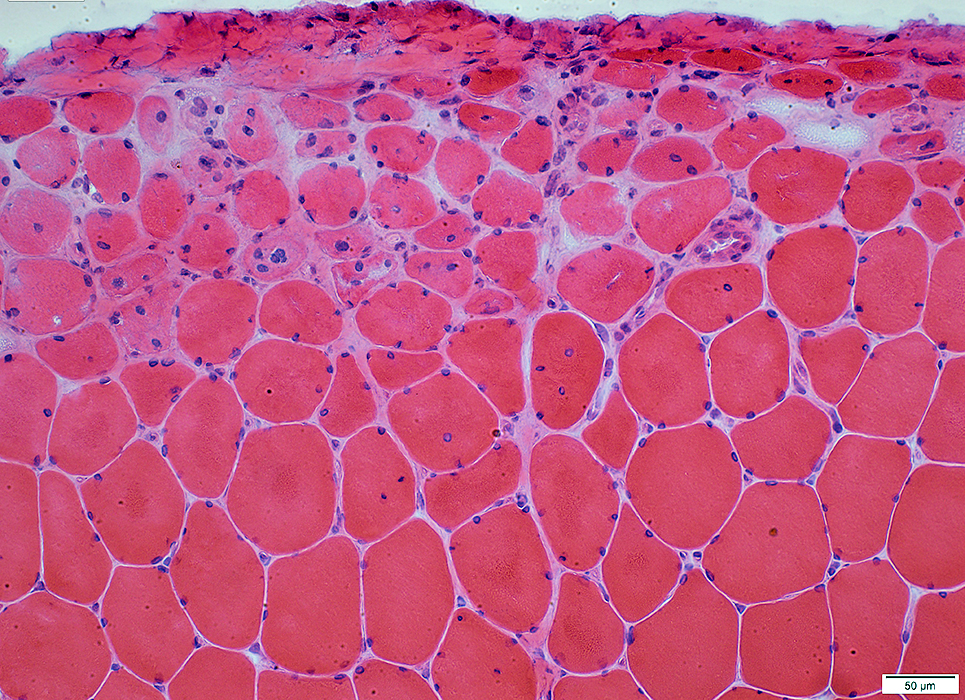 H&E stain |
Nuclei: Enlarged: Internal
Muscle fibers: Intermediate size
Endomysial capillaries: Large
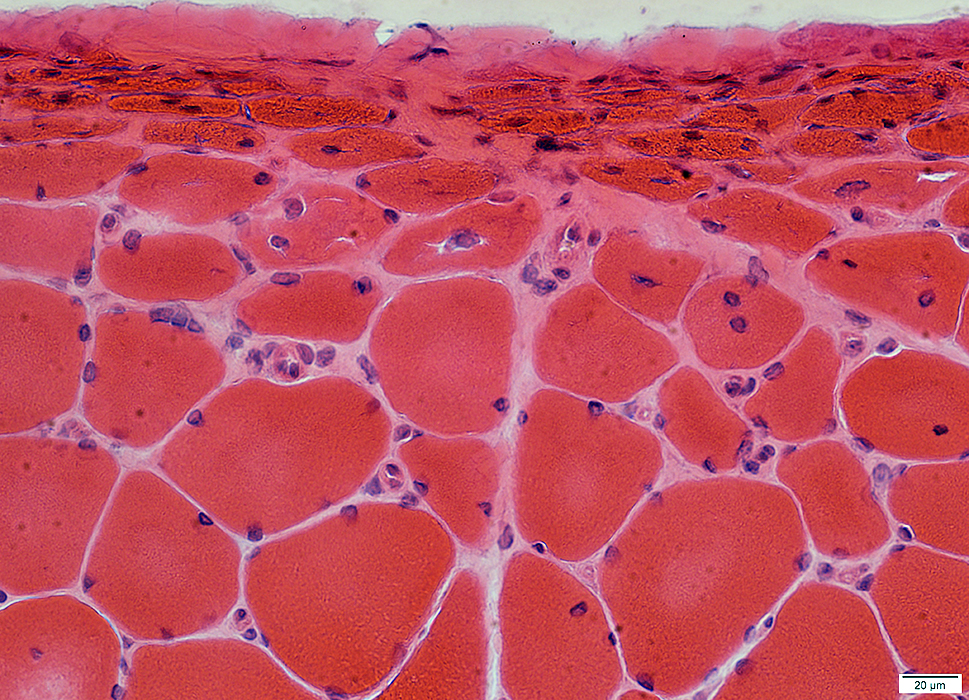 H&E stain |
 Gomori trtichrome stain |
 VvG stain |
 Congo Red stain |
Internal Architecture
Smallest muscle fibers: Very dark stained
Intermediate-sized muscle fibers: Irregular staining & aggregates
Endomysial capillaries: Positive staining
 NADH stain |
 Cytochrome oxidase stain |
Muscle fibers in, & near, region of atrophy have reduced COX
Muscle fibers in, & near, region of atrophy have inreased SDH, diffusely, or as aggregates
 SDH stain |
Muscle fibers in purlieu zone contain aggregated, cytoplasmic material
 VvG stain |
Endomysial Capillaries: Reduced staining in regions with small muscle fibers
Some small mnuscle fibers have no adjacent capillary
 VvG stain |
DM-VP (Adult)
 H&E stain |
Lymphocyte focus: In perimysium
 Congo Red stain |
 H&E stain |
Location: Perimysium
Contents: Lymphocytes & Small vessels
 Congo Red stain |
Vessels within Lymphocyte foci
 Congo Red stain |
 H&E stain |
Small at edge of fascicles
Nuclei: Large; Often internal
Internal architecture: Abnormal; Aggregates
 VvG stain |
 H&E stain |
Small
Nuclei: Large; Often several internal
 H&E stain |
 H&E stain |
Small
Nuclei: Large; Often several internal
Internal architecture: Aggregates & Vacuoles
 VvG stain |
 NADH stain |
Small Muscle fibers: Dark stained
Larger Muscle Fibers: Sarcoplasmic reticulum aggregates
 NADH stain |
Myosin ATPase
Small muscle fibers at edge of fascicles: Reduced staining
 ATPase pH 9.4 stain |
DM-VP: MHC Class I
 MHC-I stain MHC-I Small muscle fibers: MHC-I upregulation in cytoplasm & on surface Larger muscle fibers: MHC-I mostly on muscle fiober surfaces |
DM-VP: Mitochondrial Pathology
 COX stain |
Cytochrome oxidase (COX): Reduced (Above)
Succinate Dehydrogenase (SDH): Increased (Below)
 SDH stain |
DM-VP: Aggregates in Muscle Fibers
 AMPDA stain |
 LC3 stain |
 LC3 stain |
 Acid phosphatase stain |
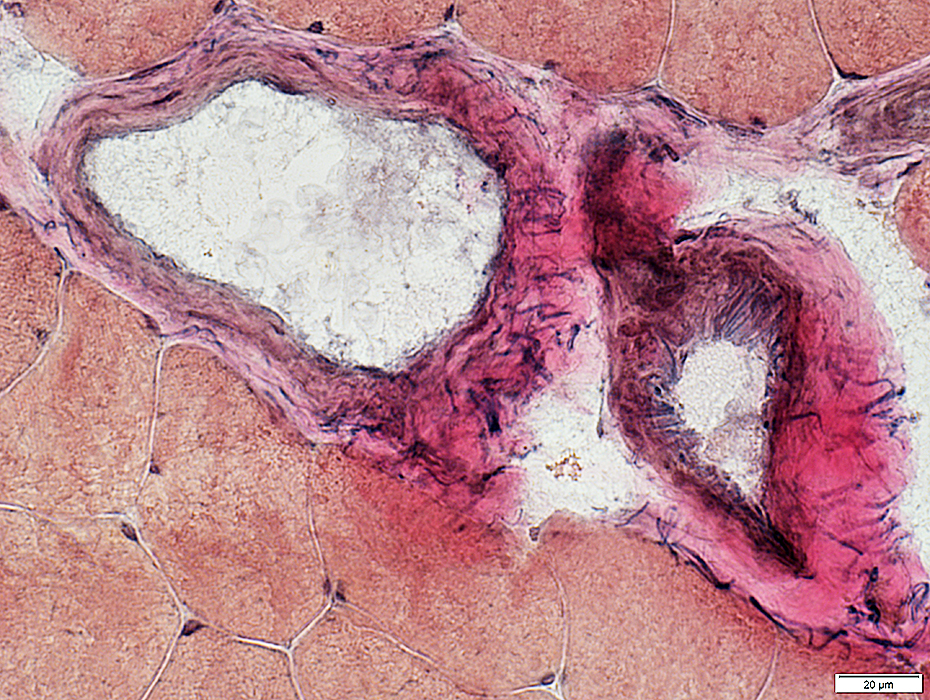
Large Artery
Abnormal structure: Patchy loss of internal fibrils
 VvG stain |
Large Vein
Abnormal; Endothelial layer is widened
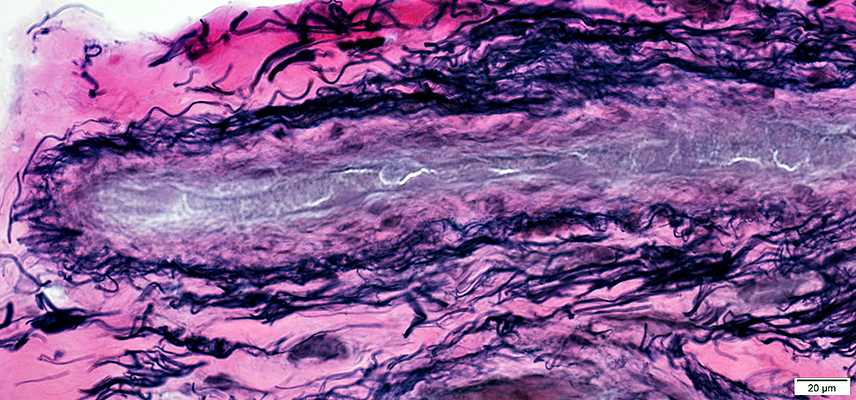 VvG stain |
Perimysial Smaller Vessel
Thick wall
 VvG stain |
DM-VP: Capillaries
 Alkaline phosphatase stain |
 UEA I stain |
Return to Neuromuscular Home Page
Return to Dermatomyositis, Adult pattern
Return to Inflammation
Return to Inflammatory myopathies
Return to Dermatomyositis
References
1. Neuromuscul Disord 2006;16:391-393
2. Muscle Nerve 2010; Online April
8/17/2022